 Back in the late 60s and early 70s, a new surgical treatment for blocked heart blood vessels was being perfected. Known as coronary artery bypass grafting, it allowed doctors to work around the heart’s own blood vessels that supply the muscle of the heart with oxygen and nutrition when they became dangerously plugged with plaque build up. Patients that previously would have most likely suffered severe or life-ending heart attacks were now being surgically repaired and at least temporarily “cured” of their heart blockages. I say temporarily, because doctors like Dean Ornish, MD, noticed that many of these patients who had undergone open-heart surgery would return several years later with new blockages in their new plumbing! Most likely, this was due to the fact that they had not changed their lifestyle and dietary habits.
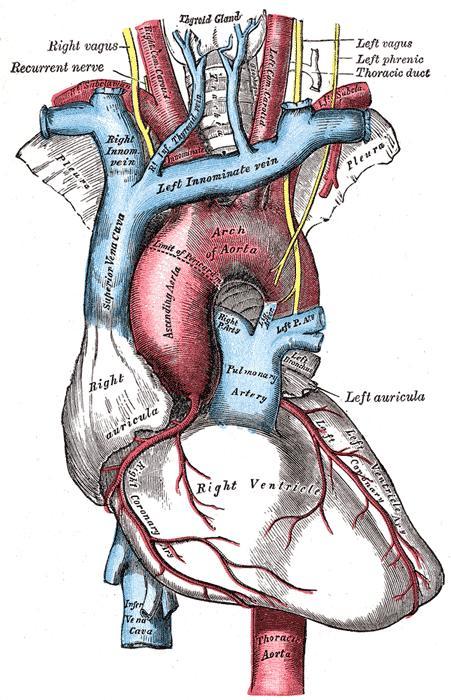
Back in the late 60s and early 70s, a new surgical treatment for blocked heart blood vessels was being perfected. Known as coronary artery bypass grafting, it allowed doctors to work around the heart’s own blood vessels that supply the muscle of the heart with oxygen and nutrition when they became dangerously plugged with plaque build up. Patients that previously would have most likely suffered severe or life-ending heart attacks were now being surgically repaired and at least temporarily “cured” of their heart blockages. I say temporarily, because doctors like Dean Ornish, MD, noticed that many of these patients who had undergone open-heart surgery would return several years later with new blockages in their new plumbing! Most likely, this was due to the fact that they had not changed their lifestyle and dietary habits. As early as 1977, cardiologists started trying to treat the blockages in the heart blood vessels without having to crack the chest open, but, instead, threading a catheter into a large blood vessel in the groin area and guiding it up to the heart and into an individual heart blood vessel. Once at the narrowing area of the blood vessel threatening the patient’s heart, a small mesh scaffold, called a “stent,” was slipped into place and gently expanded to reopen the narrowing. This stent was then left in place.
All this history gets personal for both Nina and me, as we both have had loved ones undergo stent placement for coronary heart disease in the past year. In my case, my family member had just celebrated his 50th birthday, and with little prior warning or symptoms, had a sudden cardiac event at home that required CPR and electric shock to the chest by the EMTs to restart the heart beating again. Evaluation at the hospital immediately afterwards showed one heart vessel with a blockage and a stent was put in place right away. Follow-up tests showed no permanent damage to the heart muscle from this heart attack—thank goodness!
It has been found that patients who go through “cardiac rehabilitation” programs following stent placement do better down the road than those that don’t. Cardiac rehab involves progressive aerobic activity on treadmill and stationary bikes while having the heart rhythm monitored, for 30 minutes 3 times a week for 3 weeks, then bumped up to 45minutes, 3 times a week for 3 more weeks. In my family member’s situation, he had been very physically active prior to his event, swimming and golfing regularly, and he was anxious to be able to return to those activities. If yoga had been his thing, I suspect that same desire would have been there. So, what are the recommendations about “return to activity” that could guide you as a yogi if you have to have a stent placed? The NIH has the following post-stent recommendations:
“After a stent procedure, [because of the risk of blood clots causing your open vessel to close,] your doctor will likely recommend that you take aspirin and other anticlotting medicines. Patients are told to avoid vigorous exercise and heavy lifting for a short time after the stent procedure. Your doctor will let you know when you can go back to your normal activities. …However, stents aren't a cure for atherosclerosis or its risk factors. Lifestyle changes may include changing your diet, quitting smoking, being physically active, losing weight, and reducing stress. You also should take all medicines as your doctor prescribes. Your doctor may suggest taking statins, which are medicines that lower blood cholesterol levels.”
Interestingly, there aren’t many other warnings I could find about returning to full activities, such as yoga, and no specific warnings about avoiding certain positions, including inverted yoga poses. In fact, a student of mine had his first of four stents placed for angina, or heart pain, starting at age 67 in 2000. He started doing yoga in 2003, which included regularly practicing Shoulderstand (Sarvangasana) at the wall in his new home yoga practice. He has continued to include it since then. He felt pretty certain he had discussed doing yoga with his family doctor at the time, as well as his heart doctor, and was not given any specific restrictions or warnings about yoga in general.
I would not suggest that this means you should start a vigorous yoga practice that includes a lot a challenging inversions, but would instead suggest a gradual introduction of yoga over the course of time, just as the cardiac rehab is gradually advanced while monitoring for worrisome symptoms. And certainly engage in a conversation with your heart doctor about their views on the safety of your desired yoga program. Also, keep in mind that even a gentle yoga practice, like the one used in the Ornish Heart studies, has been shown to have powerful effects on long term heart health. So you likely have a wide range of options as to the kind of yoga practice you might restart or start for the first time if you find yourself confronted with a new diagnosis of coronary heart disease. If any of our readers have been given different advice by their docs, please write to us about it.
Subscribe to YOGA FOR HEALTHY AGING by Email ° FollowYoga for Healthy Agingon Facebook

