I received this email a while back, and at first I thought someone was pulling my leg!
"I have a family member who was recently diagnosed with Proctalgia fugax. I was wondering if you could tell me if there are any ways that yoga can support preventing and dealing with flare ups of this."
You see, because "proctalgia fuguax" means pain in the rectal area, I read this as “I have a family member who is a pain in the rear….” But then I realized it was not “is” but “has”! Proctalgia fugax (PF) is a condition of pain in the rectal area that you might not think is super common (there might be some reluctance for many patients to come forward with the condition due to embarrassment) but it turns out the prevalence ranges from 6-18% of the population of the developed world. And a very unwelcome guest it is when someone develops it.
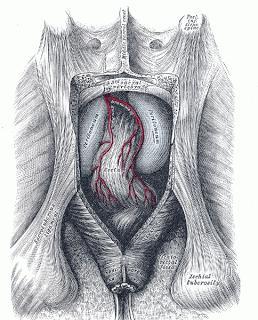
The posterior aspect of the rectum exposed
by removing the lower part of the sacrum
and the coccyx
The underlying cause is not clear, although spasm of the pelvic floor muscles is at the top of the list of possibilities. There is a theory that there is some connection to Irritable Bowel Syndrome, and high levels of stress also seem to aggravate PF and LAS, just like IBS. Episodes of pain can happen both day and night, and since the symptoms don’t last very long, most western pharmaceutical treatments to treat the pain once it arises are not very effective.
Patients with PF or LAS will have unpredictable, episodic pain. It can start in a person’s teen years, but often appears during adulthood, the average of onset being 45. More women than men report it, but that may be because women actually report things to their doc. Come on, fellas—fess up! And because there could be another more serious condition causing pain in the rectal and anal area, it is important to have a visit to your doctor to rule out more serious and potentially life-threatening conditions. Once that is done, you can feel more reassured that this is ultimately a benign condition, but one you may be able to improve with yoga tools.
Just as IBS has been found to improve with regular yoga practices, I think PF may also. There is no formal research on this, so your family member can study his/her own symptoms and see if the yoga practices lower the frequency, intensity and duration of pain episodes. As is almost always the case, start with gentle, beginning-level poses, and add in simple quieting pranayama practices and meditations that promote deep physical and mental relaxation. From there, you could see what effect adding the practice of simple inversions like Downward-Facing Dog, Legs Up the Wall (Viparita Karani) with the hips elevated, and Supported Bridge Pose on a block, will have on the PF symptoms. I postulate that the inversions will decrease the blood pressure and general pressure from the pelvic floor, which could have a beneficial effect on the PF course.
According to the Columbia University’s Health website’s Q&A pages:
"The most common treatment for Proctalgia fugax is simply to push on or massage the anal area or the perineum. This may be done manually, or by straddling the edge of an empty bathtub (carefully) or sitting on a tennis ball."
And an old research report from 1961 mentioned that several members of a family that had several generations of family members who had PF symptoms would sit with the heel for one foot under the perineum when pain struck, and it seemed to relieve the pain. This sounds like the foot position taught in the Iyengar tradition for some of the seated poses like Ardha Matsyendrasana. The heel in the perineum is also mentioned in the earliest books on hatha yoga, not to relieve pain but to influence prana in the body. How intriguing that it could also relieve pain! Might be worth practicing this when the pain strikes.
Since this is relatively uncharted territory as far as yoga’s influence of Proctalgia fugax goes, please let us know if introducing yoga has some effect on your relatives PF! For more details on PF and LAS, check out this website about proctalgia and rectal pain from the UK.

