For women that have multiple children, often weight gain between pregnancies can increase the risk of developing diabetes. By having an opposite effect, it appears losing weight between the third and fourth pregnancies appeared to reduce gestational diabetes mellitus (GDM) risk inside a second pregnancy, particularly for ladies who were overweight or obese to start with.
Approximately 7% of all pregnancies are complicated by GDM, leading to more than 200,000 cases annually. The prevalence may vary from 1 to 14% of pregnancies, depending on the population studied and also the diagnostic tests employed.
Based on the American Diabetes Association, GDM is understood to be any degree of glucose intolerance with onset or first recognition during pregnancy. The meaning applies whether insulin or only can be used for treatment and set up condition persists after pregnancy. It doesn’t exclude the possibility that unrecognized glucose intolerance might have antedated or begun concomitantly using the pregnancy.
Pregnancy Weight Gain and Your Health
Seem like you’ll have to start buying the Snickers in king-size (and bulk)? Actually, that recommended pregnancy weight gain isn’t your ticket to Candyland, but instead a prescription for smart, healthy eating which will lead to good, healthy weight gain. So before you decide to dig in, keep in mind that pregnancy weight gain is a delicate balance – gaining an excessive amount of weight during pregnancy can lead to complications and health issues for you and your baby, however the same goes for not gaining enough weight during pregnancy, too.
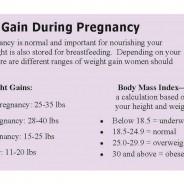
That’s why it’s vital that you talk to your doctor about how exactly many pregnancy pounds you need to pack on. Since every pregnant woman differs, there’s no “one-size-fits-all” magic number. That 25-to-35-pound recommendation fills the balance for a healthy woman who’s carrying one baby and what food was in her ideal weight before she conceived – and (surprise!) a lot of women don’t fit that description. Quite simply, don’t be shocked if your practitioner “assigns” you pretty much than that average range.

Pregnancy Weight Gain
And since you’re dining for two, make certain you’re eating well during pregnancy – and frequently! Instead of three meals a day, try switching to 6 mini meals and snacks that fuel you and your baby (this will help you fight pregnancy fatigue). Picking munchies full of protein, nutrients, and complex carbs can help you gain those pregnancy pounds the healthy way (plus keep your blood sugar steady).
Good Nutrition During Pregnancy
What and just how much should you eat to become healthy during pregnancy? You need to pay special focus on certain nutrients and add about 300 extra calories to your diet. The typical recommended daily caloric intake varies based on your activity level and normal weight. Your weight gain is a great guide to how well you’re meeting your caloric intake.
Protein
You need to increase your protein intake to 60 grams during pregnancy to maintain the growth of your baby and your breasts, uterus, and placenta; for that increased blood volume; but for the production of amniotic fluid.
Iron
Iron is a vital nutrient during pregnancy for three primary reasons. First, iron is essential for the formation of maternal and fetal hemoglobin, the oxygen-carrying element of blood. Since your blood volume increases considerably during pregnancy and your baby is manufacturing blood cells, too, your requirement for iron increases. Second, over the last trimester, your baby draws of your stuff some of the iron reserves which help prevent anemia during the first four to 6 months of your baby’s life. Third, your increased blood volume and iron stores help your body adjust (to some extent) to the blood loss that occurs during childbirth.
If your doctor recommends an iron supplement, it’ll probably contain 60 milligrams of iron, even though the recommended amount during pregnancy is 27 milligrams each day. Because iron from supplements isn’t totally absorbed, you have to ingest about 60 milligrams of iron to actually actually absorb the recommended daily quantity of 27 milligrams.
Iron supplements would be best absorbed if taken with foods full of vitamin C, such as orange, grapefruit, or tomato juice. Absorption is impaired for them with antacids or calcium-containing foods, for example milk and cheese. Iron supplements sometimes cause an upset stomach, constipation, or nausea. If that’s the case for you, keep in mind that you can get much of the iron you require from iron-rich foods, such as organ meats, red meat, egg yolk, and legumes (dried peas and beans). Consult your doctor before stopping an iron supplement, however.
Calcium
During pregnancy, many doctors commonly suggest that you get between 1,200 and 1,500 milligrams of calcium each day. Calcium is essential for that development and development of your baby’s skeleton, heart, muscles, and tooth buds. Inadequate intake leads to depletion of your own stores of calcium.
Milk and dairy food (such as yogurt and cheese) are the most useful sources of dietary calcium. Tofu and canned whole fish (with bones) are great secondary sources. If you’re lactose intolerant, meaning you can’t digest the lactose present in milk products, try a reduced-lactose or lactose-free milk product, soy milk, acidophilus milk, buttermilk, or cultured yogurt. If everything else fails, your doctor may suggest a calcium supplement.
Vitamins
The recommended daily consumption of nearly all vitamins increases 25 to 50 % for pregnant women. The daily recommendation for folic acid (Folate) doubles. A high-quality, varied diet will give most of the vitamins you’ll need, with the probable exception of folic acid. Folic acid supplements of 400 micrograms are often recommended to provide for the elevated folic acid requirement.
Folic acid is important for synthesis of cells and for manufacture of DNA and RNA, the inspiration of cells. Deficiency may cause megaloblastic anemia (development of abnormal red blood cells) within the mother and neural tube defects within the fetus.
Since adequate folic acid intake is really important for your baby and also you, choose a diet high in foods containing this essential vitamin. Liver, lean beef, legumes, egg yolks, and green leafy vegetables are great food sources of folic acid.
