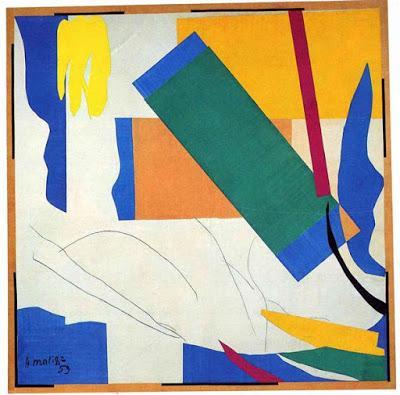
Memory of Oceania by Henri Matisse
Baxter: To date, there has been very little research focused on cognition and memory in Parkinson’s disease and yoga. What has been your personal experience with how yoga can affect cognitive function and memory?Richard: As soon as you’re diagnosed with Parkinson’s disease (PD), if you’re not already a yoga student, get yourself to a yoga class. I should be clear though, not just any class, certainly not any of the so-called “flow classes.” This isn’t a criticism of that style. But with PD, you’ll need to hold the pose for a goodly length of time to receive its fullest benefits, which means ideally the teacher should have some training in the use of props. You’ll also want to have a home practice, so that you’re at work/play at least four days a week, for at least 30 minutes each time. As far as mental fitness, cognition, and memory goes, because of the limitations imposed on my body by this condition (be sure not to label it a “disease”), I’ve had to slow my practice way down, to linger in certain positions well beyond the time I was once accustomed to (thus, the need for props). Is there a silver lining? It’s taught me to slow down in general and look at people and things in the world more intently, so that I now feel in some respects more involved in my life, more aware of myself moving through the day, and more open to other people. Memory, short-term at least, will tend to worsen over time, so that slowing down and being more aware in the present will help to counter some of the absent mindedness (I also have to take into account my age–69–and some less than healthy habits in my youth).I also feel for mental fitness that it’s useful to have some kind of meditative practice. I should qualify that word “meditative” because it’s not exactly right. I considered my breathing practice the equivalent of meditation. My “meditation” practice took the form of learning something very difficult for me, to wit, Sanskrit. I actually participated in a class for 18 months (with a slowly diminishing enrollment, until after that year-and-a-half what started out with 15-18 was down to 2 of us), and when the teacher left for India, I hired a Cal teacher who I studied with for 2 years. Moving, too, can be a meditative practice. I’ve been practitioner now for 36 years, which means I’m in very close contact with all parts of my body. When I’m walking down the street and the Parky shuffle takes over, I simply “pretend” that nothing is happening and mimic normal walking. The biggest boon for mental fitness is the breathing practice. One of the symptoms of PD is anxiety and depression. Here’s an anecdote you can share. I was seeing a psychiatrist maybe 10-12 years ago, and to help me deal with my depression (probably a mild case) she prescribed some anti-depressants. Off I went to the pharmacy to have it filled, and as I was waiting I decided I’d treat myself to a candy bar. When I went up to the counter to claim my meds, it turned out that the candy was almost as expensive as the meds. It occurred to me these pills were being passed around like candy, and right then and there I decided I wasn’t going to take them. I began instead a breathing regimen, and within a relatively short time the worst of the depression had passed. I want to emphasize that by this time I’d been yoga-ing for more than 20 years, so I had at least some sense of what I needed to do. I also want to emphasize that my condition is relatively benign. I don’t know if the breathing would have the same effect if the PD had hit me hard. Be sure though not to over-practice any of the heavy breathing techniques, the wrong breath can exacerbate matters considerably….Baxter: Can you expand on your recommendations for pranayama? Richard: Practice lengthening the exhalation, for sure. Start by just watching the breath, nothing else. If the brain refuses to quiet down somewhat after 5 minutes or so, then probably do nothing more than observe. The old texts are clear, no conscious breathing without a sattvic mind (balanced, clear)—good advice. Then, count the length of few exhalations to get an average length, and when ready to begin, add 1-3 counts to that number. Some folks, however, get disturbed by the counting, so use it judiciously. Then, once the longer exhalation is established, begin to observe the brief pause preceding the inhalation. When ready, elongate the pause (but not a hold) while waiting for the next inhalation to arrive. Think of "receiving" the inhalation, not "taking" it (nostrils stay soft, not flared, brain resting on occiput). I might put a light weight, such as an eye bag, on the sternum, so after it raises on the inhalation, the breather lowers it slowly trying to keep as much lift as possible during the exhalation. Also (for depressives) rather than lying on the usual support, you might try lying on a rolled up washcloth positioned opposite (behind) the sternum. That gives just enough push to the chest to encourage expansion but not so much that the inhalation becomes a strain. I might also use foam earplugs, they amplify the sound inside the skull, which then becomes a handy way to monitor the quality of the breath, making the sound of the inhalation/exhalation even from beginning to end. It is very important then to monitor the emotional reaction. At the first sign of trouble, STOP, go to Savasana (Relaxation pose). Generally, the quality of attention to the breath is more important than the length of practice. One problem: people with PD often suffer from insomnia, so quality attention is difficult, and the brain tends to wander easily. If the person is serious about using the breath as a healing modality, then persistence is called for, continually returning to the breath. And it usually gets easier to stay focused over time. But its also important not to expect too much too soon—there’s no timetable, be patient with yourself. Maybe later once the reclining practice is established, try adding in work with the nadi’s (yogic energy channels). Go whole hog with weight on the thighs, and I like 1 lb. lead fishing weights on my palms. Need help with yoga and PD? If Baxter can't answer your question (not at all likely), feel free to email me at: [email protected]Baxter: Thanks for that amazing information, Richard! I am certain our audience will find it very helpful. If you want to learn more about pranayama, check out Richard’s two books on the topic The Yoga of Breath and Pranayama and Beyond the Fundamentals, or his new book Yoga FAQ, which I reviewed here.If you want to catch my live webinar "Yoga for Your Brain” on Yoga U Online tonight (Tuesday, February 28), which includes some of this information about yoga and Parkinson’s disease, here is the link, http://us5.campaign-archive2.com/. You can use the code BBYOGA15 for a nice price discount.Subscribe to Yoga for Healthy Aging by Email ° Follow Yoga for Healthy Aging on Facebook ° Join this site with Google Friend Connect

