In my “day job” as a home health physical therapist, I see a lot of clients who have significant breathing difficulties. One of the most common breathing ailments is Chronic Obstructive Pulmonary Disease (COPD). COPD is similar to asthma in that some of the symptoms are the same but the etiology of the disease is different. Most significant is the inability to get air out and not being able to get enough oxygen in.
Let me give you a bit of background about breathing and normal airways. Air travels into the lungs via the trachea. It goes down a series of branching airways called bronchi. These bronchi branch into smaller bronchioles and then into millions of tiny air sacs called alveoli. Oxygen in the air passes through the thin walls of the alveoli into the tiny blood vessels nearby, attaches to red blood cells and is carried into the blood vessels to the rest of the body. Carbon dioxide is passed out into the alveoli from the red blood cells and is breathed out. But breathing doesn’t always depend upon the oxygen needs of the body. Breathing can be related to emotions, body tension, sensations of pain, pleasure, and body movements.
Breathing is composed of two main parts: inhalation and exhalation. Inhalation is the process of taking air into the lungs. It can occur with different amplitudes or volume of air. It can occur at a variable rate, and it can be less active. Exhalation is the process of letting air flow from the lungs back outside the body. It can vary in amplitude, rate and effort. You can stop your breathing but, of course, not permanently.
There are two main types of breathing: costal (ribs) breathing and diaphragmatic breathing. In costal breathing the ribs open and close primarily and in diaphragmatic breathing the abdomen changes shape.
The volume of air that one breathes in inhalation is called “tidal volume” and in rest or relaxation it is at a minimum. When we do moderate activity, we increase the amount of air that is bought into the lungs but this doesn’t change the tidal volume. When we maximally exhale the air from our lungs, there is always some air left in the lungs and this is called residual volume.
Other factors that influence the depth of our breath include rib cage flexibility, (the more flexible the rib cage, the more we can increase the amplitude of our inhalation) and muscular strength of the muscles of exhalation. The diaphragm is the primary muscle of inspiration. The secondary or accessory muscles of respiration include many muscles of the ribs, neck, chest wall, and trunk (abdominal muscles).
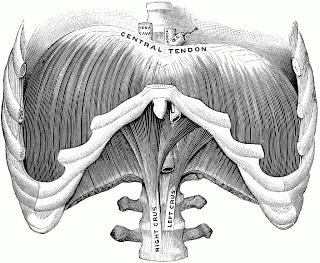
The Diaphragm (with ribs cut away)
When we breathe, the diaphragm contracts and moves downward if the abdomen is relaxed. The belly will then gently expand outward and the lower regions of the lungs expand downward. When we exhale, the diaphragm relaxes and moves back up, the belly moves in a bit.An individual with COPD works very hard to breathe. Often there are postural changes that occur over time that may be structurally compromising the ability of the rib cage to expand and return to resting position. If the anterior chest wall is collapsed and tight, then we don’t have the rib or thoracic flexibility to encourage the lungs to fill to their capacity. Breathing involves muscles, skeletal and joint articulations and is an interface of organs and movement. But breathing is also an emotional activity.
Because an individual with COPD is chronically short of breath, they fear movement because it makes them short of breath, so in turn they become chronically deconditioned, and weak due to immobility. The fear of not being able to breathe leads to increased anxiety, depression and more fatigue and stress. Here is where the practice of therapeutic yoga can be so beneficial for an individual with COPD.
If we consider the individual fully and address their physical, emotional, neurological and spiritual nature, we can assist them in learning to move again within the confines of managing their respiratory issues. Learning to observe one’s breathing pattern and to gently try to increase the exhalation compared to the inhalation is quite beneficial for someone with COPD. Gentle asana practice that addresses areas of chronic tightness and postural awareness with improved skeletal flexibility allows more freedom of respiratory movement. Please see all our wonderful prior posts for gentle seated practices and safe gentle yoga poses. Also please reread the pranayama posts because these can be adapted to a COPD breathing pattern if the emphasis is on the exhalation with no retention holds at either the end of inhalation or exhalation. Lastly, trying to walk with good self pacing and breathing awareness (sort of like a meditation practice) is a wonderful way to begin to address the poor endurance that plagues someone with COPD. If you yourself have COPD or know someone with COPD who wants to study yoga, I would recommend individual private one-on-one yoga sessions to start, and then, if and when possible, moving on to a gentle yoga class that is slow paced.
Note: November 16, 2013, Shari and her colleague, Bonnie Maeda, will be teaching a workshop in Brentwood, California on Yoga for Breathing and Sleep Apnea, which covers COPD and other topics. For further information or to register for the workshop, see brentwoodyogacenter.com.

