Have you noticed that your blood sugar rises first thing in the morning? Is your morning glucose reading sometimes your highest at that time of the day? If so, you are not alone.
As low-carb diets and intermittent fasting become more popular, more people experience the so-called "dawn effect" or "dawn phenomenon." But why does it happen? And, more importantly, is it anything of concern?
This guide will walk you through the science behind the dawn effect, focusing on what we know and what we don't know as it applies to low-carb nutrition.
What is the dawn effect?
The dawn effect simply refers to an unexpected increase in fasting blood sugar, usually upon waking. This phenonmenon was first noted in patients with type 1 diabetes in the 1980s. It was defined as rising blood sugar without the usual compensatory rise in insulin.
As morning approaches, the body naturally increases glucose production. However, the insulin the patients took the night before was insufficient to control the glucose rise. The mismatch led to an increase in serum glucose.
Researchers determined the early morning glucose rise was from an increase in the so-called "counterregulatory hormones" cortisol, epinephrine, and norepinephrine.
These counterregulatory hormones stimulate the liver to secrete glucose into the body. But, if someone has a normal insulin response, the insulin level rises appropriately to ensure the blood glucose level remains stable.
Instead, the extra glucose is taken up by the cells and used for energy. You can think of this as the body preparing itself for the increased energy demands needed for waking up and ensuring enough glucose is ready for use.
Studies in people without diabetes show the body increases insulin secretion between 4 am and 8 am. This extra boost of insulin acts to stabilize blood glucose levels.
Therefore, for decades, the dawn effect has been assumed to only be a problem for those with type 1 or type 2 diabetes. But now, that thought process may be changing.
Implications
For people with diabetes, a prominent dawn effect signifies an inability to control morning blood sugar and may have long-term health consequences.
One study showed the dawn effect is associated with a 0.4% (4 mmol/mol) increase in hemoglobin A1c (HgbA1c) levels.
Since higher HgbA1c levels correlate with a higher risk of complications, the dawn effect likely has harmful health consequences for those with diabetes. The current recommendations is to aggressively treat the dawn effect with medications to improve overall glucose control.
But what if someone doesn't have diabetes? Or, what if they follow a low-carb diet and preferentially burn fat for fuel instead of glucose? Would the dawn effect have the same implications? We'll explore that next.
The dawn effect in fat burners
First comes the bad news. We are not aware of any scientific studies that look at the dawn effect in individuals who follow a very low-carb diet.
However, based on clinical experience, the dawn effect is relatively common among those following a ketogenic diet.
Remember the physiology. As you get closer to waking, your body secretes counterregulatory hormones, which increase the liver's glucose output. But if the glucose rises, that implies the compensatory rise in insulin is not present. Why would this be?
Again, we don't have concrete evidence to explain why blood sugar rises, but we have theories.
One theory is that the pancreas does not need to respond quickly to elevated blood sugar since it rarely happens on a very low-carb diet. In essence, the feedback loop rebalances.
Another theory focuses on muscle cells. Under glucose burning conditions, muscle cells are the prime driver of glucose uptake, taking glucose out of the blood to be used for energy.
However, when your cells instead burn fat for fuel, as they do in nutritional ketosis, the muscle cells don't need glucose. The brain, on the other hand, still needs some glucose. Muscle cells become "resistant" to glucose so that the brain can preferentially have access to glucose.
Many call this physiologic process "adaptive glucose sparing" or "physiologic insulin resistance." The idea is that the lack of glucose uptake happens for a beneficial reason, not a harmful reason, as it does in diabetes. Again, this is a theory, but it is a theory that makes physiologic sense.
Some believe insulin resistance provided an evolutionary advantage for our hunter-gatherer ancestors, allowing us to utilize glucose in our brains and allow our muscles to run on fat.
One potential key is the presence or absence of insulin resistance. Elevated glucose in the setting of insulin resistance has a different physiology than the same glucose in the presence of insulin sensitivity.
While that does not mean the two situations have different outcomes, the physiologic difference suggests they might.
Is the dawn effect always harmful?
While research suggests the dawn effect is potentially harmful to those with type 2 diabetes, can we say the same for those without diabetes?
Without research to guide us, we have to use our best reasoning skills to reach a hypothesis.
Blood glucose appears to exert harmful effects in two ways. One is when glucose is chronically elevated, and the other is when glucose has large increases or "spikes," known as the glucose variability.
Both mechanisms have been shown to accelerate vascular and endothelial dysfunction.
Therefore, we could conclude that if neither of these concerns is present, there is no chronic elevation and the rise is relatively small, then there should not be concerning consequences.
How do we measure or define "chronic elevation?" That is usually measured by the hemoglobin A1c (HgbA1c), roughly the 3-month average of blood sugar. The higher that is, the higher the average blood sugar. It isn't perfect, but it is a surrogate for chronic blood sugar elevation.
However, the HgbA1c may not account for shorter, more intense blood sugar elevations, the so-called glycemic variability.
A postprandial glucose increase up to 140 mg/dl (7.8 mmol/L) is considered normal.
Therefore, we may be able to infer that a dawn effect up to 140 mg/dl (7.8 mmol/L) should not be a cause of concern.
This is especially true if it is the highest level of the day, and postprandial levels are significantly lower. Again, there are no data on this, so it is our hypothesis. But it makes sense.
Based on this theory, if the HgbA1c is in the normal range or improving, the dawn peak blood glucose level is less than 140 mg/dl (7.8mmol/L), and postprandial elevations even lower than 140 mg/dl (7.8mmol/L), then it seems reasonable that the dawn effect is not a major clinical concern.
However, if these criteria are not met, then we have to wonder if the morning elevation is adding to an ongoing problem.
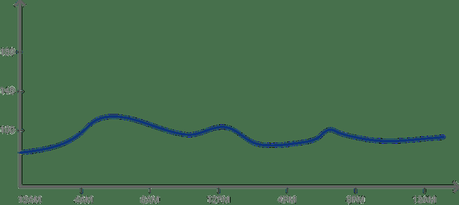
As an example, here is a representation of a continuous glucose monitor (CGM) graph that would suggest less of a risk for a dawn effect. Notice the peak is at 120 mg/dl (6.7 mmol/L), and it is the highest level of the day, with postprandial rises staying below 110 mg/dl (6.1 mmol/L) and returning to baseline within an hour.
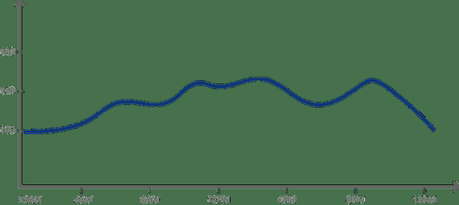
On the other hand, this graph suggests that the dawn effect is part of a larger problem. The blood sugar starts high, with a peak of 130 mg/dl (7.2 mmol/L), and it never gets back to baseline before rising again to well above 140 mg/dl (7.8 mmol/L) after the subsequent two meals.
These two graphs differ in the following ways:
- The degree of blood sugar elevation
- The chronicity of elevation
- And, they suggest different underlying mechanisms for the blood sugar rise
Can you decrease the dawn effect?
As we discussed above, the dawn effect may not be a concern. But if you feel it could contribute negatively to your health, what can you do to lessen it?
- Exercise may help. Doing some form of physical exertion after dinner and first thing upon waking may reduce the degree and duration of the glucose increase.
- Also, eating early in the morning can help reduce the dawn effect. This may seem paradoxical. Wouldn't eating raise blood sugar? Not in this case.
Remember, the dawn effect is due to lower than usual insulin secretion in the morning to make sure you have adequate available glucose. If you take in food, that will signal your body that you have adequate energy and your insulin may respond appropriately. The result is more insulin to help bring down your glucose level.
- Some people recommend eating a high-fat or high-protein snack before bed to minimize the dawn effect. I would suggest keeping this as a last resort, as the potentially negative effects of late-night snacking likely outweigh any benefit of a mild reduction in the dawn effect.
- Don't forget the importance of sleep! A poor night of sleep can increase cortisol production, leading to an increased dawn effect.
- Lastly, some may consider the use of medications. Taking insulin in the evening tends to be more effective than oral diabetes medications at reducing the degree and time span of glucose elevation.
All medications, especially insulin, have potential side effects, including the risk of dangerously low blood sugar. You should discuss any potential medication change with your healthcare provider and have a thorough risk-benefit analysis.
Summary
We know a great deal about the dawn effect as it relates to diabetes and the increased risk for potential complications. However, we know much less about the dawn effect in people following a low-carb diet whose muscles primarily burn fat rather than glucose for fuel.
Based on what we know, we can extrapolate conditions that may or may not signify concerning parameters for a dawn effect.
For many, the mild morning blood sugar rise is likely a physiologic adaptation that is not a health concern. But until we have scientific proof, you should investigate your morning blood sugar elevations with your healthcare professional and consider available tools to address it if needed.

