Can obesity cause diabetes or cardiovascular disease? And if not, how are they related? These are questions looking for answers, and a small piece of the puzzle fell into place last week.
A new systematic review and meta-analysis, published in JAMA Network Open, is the first-ever meta-analysis pooling data from studies conducted with a technique called Mendelian randomization which employs genetic markers and number crunching to mimic a clinical trial.
Cleveland Clinic Newsroom: Cleveland Clinic genetic analysis links obesity with diabetes, coronary artery diseaseMendelian randomizations are less reliable evidence of causation than randomized clinical trials, but they are much less expensive to conduct, and are better evidence than observational studies. The study authors explain:
Mendelian randomization offers an opportunity to study associations without many of the typical biases that are inherent in traditional epidemiologic approaches. Thus, Mendelian randomization can fill the evidence gaps by minimizing confounding, if variables are randomly and equally distributed in the population of interest.
What did the investigators find?
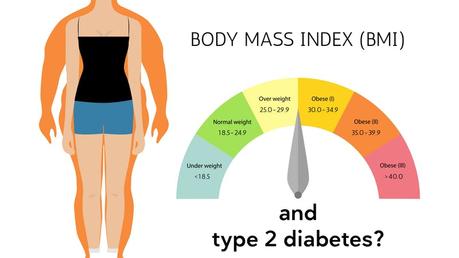
In this systematic review and meta-analysis of nearly 1 million participants, obesity was associated with type 2 diabetes and coronary artery disease but not with stroke... Meaning that obesity may increase the risk of subsequent diabetes and may contribute to cardiovascular outcomes and should thus remain a major focus of public health initiatives.
More specifically, each five point increase in BMI increased the relative risk of a type 2 diabetes diagnosis by 67% - a substantial connection. For coronary artery disease, the association was not as strong: a five point increase in BMI increased the relative risk of coronary artery disease by just 20%. The authors of this analysis are quick to point out that Mendelian randomization studies do not prove causality. However, they do support a causal relationship.
It's a piece of the puzzle, and is consistent with the evidence called out in an editorial in the journal BMJ this week, entitled "The growing problem of diabetes." In it, editor in chief Fiona Godlee writes:
Weight loss is essential for management of diabetes and can lead to remission, but once achieved it can be hard to maintain. In what may be a ground breaking randomised trial, Cara Ebbeling and colleagues found that energy expenditure was higher when people ate a low carbohydrate diet during weight loss maintenance. People randomised to a high carbohydrate diet had higher concentrations of the hormone ghrelin, which is thought to reduce energy expenditure.
At Diet Doctor, we believe low-carb lifestyles are part of the solution to the ever-increasing global burden of type 2 diabetes. Several meta-analysis of randomized clinical trials show that low-carb regimens lower the need for blood-sugar medication while improving health markers like HbA1c and blood pressure.
Earlier
Elevated BMI tied to shorter life Is low carb the best treatment for reversing diabetes? Britain's NHS to fight diabetes with very low-calorie liquid dietGuides
How to reverse type 2 diabetes A ketogenic diet for beginners