
I have started helping patients reverse their type 2 diabetes, obesity and other lifestyle-related conditions in my low-carb clinic in February 2017. I almost always give them an extensive list of blood work to get done at the beginning, in the middle and at the end of our 6-month program. I also make them get an abdominal ultrasound and a DEXA scan at the beginning and at the end.
At every follow up visit, Nurse Sylvie weighs them, measures their waist circumference, checks their blood pressure, and looks at the blood sugar levels they have written down since the last visit. If they aim to be in nutritional ketosis, she also checks their ketonemia.
Metabolic and lipid lab tests
A good number of the lab tests that I order are very well explained by Dave Feldman on his website The Cholesterol Code, which is amazing. Dave is a senior software engineer and entrepreneur, and he's created a protocol for people whose cholesterol doesn't respond the way it normally does on a keto diet. So, you can check out the definition or reason behind certain labs here.
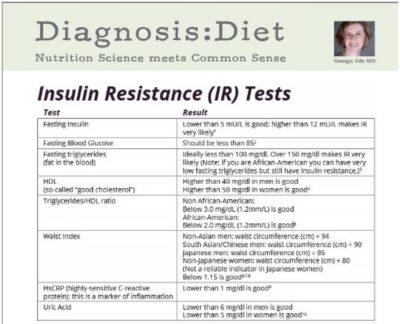
Insulin resistance lab tests
Dr. Georgia Ede's, a brilliant American psychiatrist who is passionate about the connection between food and every aspect of physical and mental health, has also put together a list of tests that can be ordered to help diagnose insulin resistance. I order every single one of them, except AST (not usually covered in my province).
Link: How to diagnose, prevent and treat insulin resistance [infographic]
Abdominal ultrasound
In my previous post, I briefly discuss fatty liver, from the point of view of a low-carb clinician. The majority of patients with type 2 diabetes and/or obesity have a certain degree of fatty liver. Liver panels alone are not enough to rule in or rule out an abnormal liver. As a matter of fact, perfectly normal ALT and AST can coexist with severe fatty liver, as reported by imaging. It's become a serious public health problem, and it's even overtaking other indications for liver transplant.
DEXA scan
It's a total body scan with very little radiation that informs us on the bone density (it can diagnose osteoporosis), lean-mass density and body-fat density. It's relatively cheap, compared to a CT-scan or MRI. The results can be surprising. We've discovered quite a few TOFI (thin on the outside and fat on the inside) patients with this imagery. I like seeing total body-fat percentages.
Glycemia and ketonemia
I always prescribe a gluco and keto meter to all my low-carb patients, with enough needles and strips to check their blood sugar levels and ketone levels as often as they want during our 6-month program. They are covered by either their personal insurance or by the government. The strips, in particular the keto ones, are not that cheap. As they progress on their low-carb journey, they require less and less monitoring.
The costs of it all
I have been told quite a few times so far by other doctors that, by ordering these tests and imageries, I am costing money to the healthcare system. Prevention is so not sexy in this day and age. Aggressive, invasive and irreversible treatments and surgeries are so much more glamorous, even when they could have been prevented by teaching proper nutrition.
It's not in the guidelines, therefore it's excessive.It won't change your treatment, therefore it's useless.
It is already known that fatty liver is likely to be found, therefore it's pointless. Knowing the actual body-fat percentage is not medically required, therefore it's not indicated. Ketosis is not necessary, therefore measuring ketones is not necessary.There is no evidence that doing an ultrasound in the obese will prevent significant disease, therefore this is not evidence based.
The reasons behind it all
Everything that we order and follow in our low-carb clinic is meant to help diagnose holistically the severity of the chronic lifestyle-related diseases that we are hoping to treat, and to help follow the progress being made. But what I consider most important, and what the patients consider most important are not necessarily the same. I particularly like fasting insulin levels (or C-Peptides), HBA1c, triglycerides and HDL. You won't be surprised if I tell you patients seem to be a lot less excited about those than I am!
Patients are particularly interested in what the scale has to say. It's one of the most potent sources of motivation. Reminding them constantly that the scale will often lie is necessary. While they don't particularly care about their ALT's or GGT's, they don't like to be told that they have a fatty liver on their abdominal ultrasound. It's a strong source of motivation too, if you have a treatment to offer them, like a low-carb diet.
DEXA scans are a good source of motivation too. No one really likes to be told that about 50% of their body is made of fat. And patients can actually picture in their minds what extra pounds of fat look like, as we all buy butter in packages of 1 pound (0.5 kg). It's concrete.

A worthwhile investment
To me, relatively inexpensive tests that help motivate patients to keep on improving their lifestyle choices are not a cost to society, but an investment.
Patients who reverse their chronic diseases and adhere to low carb for the rest of their lives will not need an increasing number of drugs in increasing doses to treat nutrition-related diseases. Anti-diabetes drugs are expensive over a lifetime.
They will likely not get the complications associated with those diseases.
Fewer visits to endocrinologists to get their diabetes drugs adjusted or their insulin started.
Fewer visits to gynecologists to treat polycystic ovarian syndrome.
Fewer visits to cardiologists because their hypertension or lipids are difficult to control, or because they are at risk for recurrent heart attacks.
Fewer visits to hepatologists because their fatty livers are turning into steatohepatitis or cirrhosis.
Fewer visits to nephrologists because their kidneys are failing secondary to type 2 diabetes.
Fewer visits to ophtalmologists because of diabetic retinopathy.
Fewer visits to oncologists for cancers related to obesity and diabetes, less visits to psychiatrists for depression and early dementia, less visits to neurologists for neuropathies, less visits to orthopedists for joint replacements and amputations, etc.
How much does it cost for one person to be on dialysis? And what about loss of productivity for society? And loss of quality of life for that person? How much does it cost when someone goes blind? Loses a leg?

It makes sense to invest in prevention.
It makes sense to help patients reverse nutrition-related diseases with proper nutrition counseling, and to support this reversal with lab tests and imageries that help this process.
-
Dr. Èvelyne Bourdua-Roy

