
Why you shouldn't blindly trust the numbers that define hypertension.
You've probably heard that 130/80 is the new threshold to hypertension. But what if I told you that this number is not based on solid science?
Meet John, a victim of the blood pressure myth.
John is a 57-year old successful entrepreneur who has been worried about his blood pressure spikes. He noticed them when he recently started to monitor his blood pressure at home. While he has been taking an antihypertensive medication, he would like to modify his lifestyle habits in the hope that his doctor might someday be able to deprescribe his meds.
The American Heart Association (AHA) has defined a systolic pressure (the upper value) of 130 mmHg and/or a diastolic pressure of 80 mmHg as the threshold above which a person should be treated for hypertension [1].
In Europe we see it a little more relaxed, drawing the “red line” at 140/90 mmHg [2].
These numbers are not magical biological thresholds above which one is doomed to die early, or suffer a heart attack, stroke, kidney or heart failure.
Yes, many studies have shown these nasty events to be associated with elevated blood pressure. But association can never prove causation.
That’s one of the statistical facts that your doctor, the associations, and the media often fail to point out.
But that’s not the worst omission. There are two more.
The Omitted Truths
First, the correlation between elevated blood pressure and elevated event risk is not as linear as it is typically portrayed.
Figure 1A represents this portrayal, 1B shows the actual data, and 1C illustrates at which blood pressure level the risk really starts to increase, based on your gender and the age at which you hit these levels [3].
Figure 1
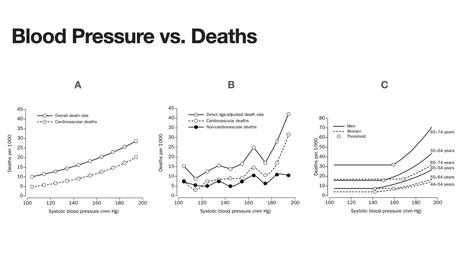
The difference between figure 1A and C is due to the statistical methods applied to interpret the raw data (figure 1B). Quite obviously 1C represents the data better than 1A.
The second, and most important, omission the purveyors of hypertension thresholds are guilty of is to hide the answer to an obvious question:
Does the lowering of blood pressure to, or below, those thresholds reduce the risk of death or cardiovascular events?
After all, the objective of treating you with antihypertensive drugs is to decrease your risk of death and of cardiovascular events.
The Cochrane Collaboration, medical science’s white knight of performing systematic reviews and meta-analyses, investigated this question.
They were interested to see whether more aggressive reduction of blood pressure (defined a reduction below 135/85 mmHg) delivers better results than treating to “standard target” defined as 140-160 / 90-100 mmHg).
“Better results” was defined to mean fewer number of deaths and of serious cardiovascular events, such as heart attack and stroke.
They pooled the data of 11 randomized controlled trials which had to meet strict selection criteria to minimize potential bias.
The trials included almost 39,000 patients and 143,000 patient years. The patients’ age ranged from 20 to 80.
Here are the astonishing results:
- There was no effect on total mortality (the risk of dying from any cause).
- There was no effect on cardiovascular mortality (the risk of dying from cardiovascular disease).
- There was no effect on kidney failure.
There were however 16% fewer heart attacks, 12% fewer strokes and 24% fewer heart failure events in the more aggressively treated groups.
That’s how these results are typically communicated to you, the patient. Those percentages sound impressive.
Here is why they are not:
The Deception With Percentages
They are relative risk reductions (RRR), not absolute risk reduction (ARR).
Let’s look at the difference:
In the Cochrane Analysis the absolute risk for heart attack was 2.5% in the group treated to standard target.
That is, of 100 people in that group 2-and-a-half (let’s be liberal and round it up to 3) suffered a heart attack.
Whereas in the aggressively treated group 2.1 suffered a heart attack (let’s round this down to 2). The ARR is 0.4% (2.5 – 2.1).
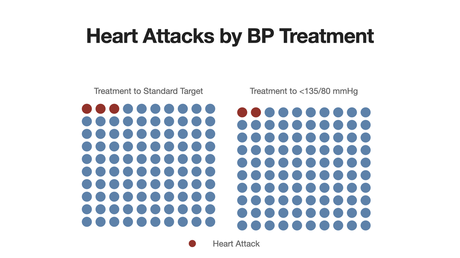
When you translate this ARR into the number of people your doctor needs to treat more aggressively to prevent one single heart attack (compared to standard target treatment), you arrive at 250.
This number is called the “Number Needed To Treat” (NNT).
Which you can express as “249 of every 250 more aggressively treated patients will not have any benefit of this aggressive treatment”.
Unsurprisingly, the Cochrane Collaboration came to the conclusion that:
“… the benefits of trying to achieve a lower blood pressure target rather than a standard target (≤ 140/90 mm Hg) do not outweigh the harms associated with that intervention.”
Coming back to John, our worried hypertensive patient. These numbers don’t tell him what to do.
That is the crux with these studies. They help health insurers and ministers weigh the commercial costs of treatments vs. their benefits.
Their “patient” is the population. They are not interested in the individual patient. But you are, and, hopefully, so is your doctor.
The Solution
That’s why John is now embarking on a N-of-1 study, in which we together turn him into a “clinical trial of 1”.
My team and I have operationalized this gold-standard method for lay-people to use. Think of it as a science kit for biohacking lifelong health and function.
John and I will be monitoring his blood pressure, and most importantly, his arterial compliance. The latter is a key indicator of vascular health.
Read more about this here.
The tools to do this are readily available. We use Withings’ WIFI capable smart scale to record daily his pulse wave velocity (PWV), and the same company’s blood pressure monitor.
Both record their data automatically into our cloud-based “science kit”.
We’ll use the arsenal of lifestyle medicine to “trial-and-error” his way to an optimal configuration of dietary and exercise habits that match his genetic predisposition. And that hopefully solves his hypertension problem.
Best of all, we can do this even though John and I live far apart.
His, and possibly your, takeaway from this post: It should put your fear of exceeding the artificial hypertension thresholds into perspective.
PS:
This post contains referral links for the Withings devices on Amazon. If you purchase the device from there, I will receive a small commission at no additional charge to you.
PPS:
If you like regular updates to my posts, follow me on LinkedIn
References
[1] Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med 2020;30:160–4. doi:10.1016/j.tcm.2019.05.003.
[2] Mancia Chairperson G, Kreutz Co-Chair R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertensi. 2023. doi:10.1097/HJH.0000000000003480.
[3] Port S, Demer L, Jennrich R, Walter D, Garfinkel A. Systolic blood pressure and mortality. Lancet 2000;355:175–80. doi:10.1016/S0140-6736(99)07051-8.

