
Insulin is an essential hormone we can't live without. What happens, however, when it is chronically too high? Our tissues stop responding to it effectively. That's insulin resistance.
Insulin resistance is a very common condition that often accompanies obesity or a diagnosis of pre-diabetes, type 2 diabetes, polycystic ovary syndrome (PCOS), cardiovascular disease, and other metabolic conditions like hypertension and non-alcoholic fatty liver disease.
Have you been told you have insulin resistance? You're not alone.
Studies estimate that up to 45% of the US population and similar numbers in other countries currently have insulin resistance. In studies of obese women, more than 70% are insulin resistant and among those with type 2 diabetes, the number rises to greater than 80%.
Many people with the condition likely remain unaware they have it.
Also concerning? Insulin resistance is being linked to cancer, Alzheimer's disease, mental health disorders and other chronic conditions.
How exactly does insulin resistance start? How do you if know if you are affected? And what can you do about it?
This in-depth guide will explain the science behind insulin resistance, help you understand why it happens and suggest the best way to get the condition diagnosed long before serious conditions like type 2 diabetes develop.
In a second, related guide, How to reverse insulin resistance, we will give you concrete steps to help your body become sensitive to insulin once more, and help prevent metabolic health problems, especially type 2 diabetes, from developing in the future.
What is insulin resistance?
Insulin resistance is when cells in your body do not respond effectively to the hormone insulin that is circulating in your body. This causes the pancreas to secrete even more of this important hormone in an effort to keep your blood sugar stable.
Insulin has many roles. Its primary role is to keep our blood sugar levels in a very tight range - called blood glucose homeostasis. That's because both too high and too low blood sugar levels are dangerous and damaging to the body. When glucose levels rise, more insulin is secreted. When glucose levels fall, less insulin is secreted. In general, keeping insulin in a low physiologic range may be better for your long-term health.
Insulin also enables glucose to be used by cells for fuel or stored as glycogen in muscle and liver cells. Falling levels of insulin let the liver know when to make more glucose (gluconeogenesis) and rising insulin levels let the liver know when to stop.
Another crucial role is insulin's regulation of fat storage. When insulin levels are high, it stimulates fat cells to take up glucose and turn it into fat (lipogenesis). Then, when insulin is low, it enables the body to take the fat out of storage and use it for energy.
For someone who is metabolically healthy, this process works seamlessly to ensure a constant supply of fuel for the body. The problem arises when we are not metabolically healthy, which some researchers estimate may be the case for as many as 88% of Americans.
When our bodies are exposed to an unrelenting supply of glucose, insulin is constantly secreted and remains chronically high - a condition called hyperinsulinemia. That is when our bodies can stop responding properly to insulin's signals.
Why does insulin resistance happen?
Genetic risk factors, environmental risk factors, and lifestyle factors such as diet and inactivity have all been found to contribute to the development of insulin resistance.
One known way that it develops is when our bodies have been bombarded by the sugar and starch in our diet for so long that our liver and muscle cells are already "full" of glucose (and it hasn't been consumed).
Since they are full, they don't want to take in any more. However, the ample supply of glucose in our blood after a carbohydrate-containing meal requires that the glucose must go somewhere. Thus, the battle ensues between our cells and our pancreas.
The pancreas secretes more insulin to tell the cells that the glucose level is too high, and they need to take in more glucose. The cells cannot respond because they are full, so they resist letting glucose enter. The pancreas then goes into overdrive, secreting even more insulin in an attempt to overcome the cellular resistance and force the glucose into the cells.
Some rightly argue that chronic hyperinsulinemia is the better term for this worsening physiologic condition rather than insulin resistance. The muscle and livers cells are not really "resistant" to insulin, it is just that they are full and cannot respond, despite the pancreas's escalating efforts. As Dr. Jason Fung has said, it's like trying to put more clothes into a completely full suitcase. The suitcase isn't "resistant" to clothes. It is simply full.
Symptoms of insulin resistance
Insulin resistance has no obvious symptoms of ill health.
The main symptom of the condition - prior to being diagnosed with pre-diabetes or full-blown type 2 diabetes - is increasing abdominal obesity for most, although not everyone will experience this.
A prevailing theory of how insulin resistance worsens is that we each have a threshold level of fat that can be stored in our adipose cells and when this is exceeded, our body starts storing fat in less ideal places - especially around the organs in our abdomen and in our abdominal cavity. This is called visceral fat and when this fat starts increasing it is the dominant sign of insulin resistance.
Other subtle signs of insulin resistance in some people are dark, dry patches of skin on the groin, armpits, or back of the neck, known as acanthosis nigricans. Skin tags - small fleshy growths - often on the neck or armpits can also be a sign of insulin resistance in some people, which is thought to occur because insulin is a stimulator of cell growth.
Other than those symptoms, most people with early insulin resistance feel fine. It is only as blood sugar finally starts to rise that other symptoms of high blood sugar and type 2 diabetes may begin to show, such as frequent urination, excessive thirst, fatigue, and excessive hunger.
It is important to understand that insulin climbs higher and higher in an attempt to keep blood sugar regulated, but the blood sugar doesn't actually rise until late in the disease process.
By the time someone is diagnosed with type 2 diabetes, they have likely had insulin resistance - or chronic hyperinsulinemia - for a number of years, perhaps even more than a decade.
Conditions associated with insulin resistance
The following health conditions are associated with insulin resistance:
- Obesity - Insulin resistance often increases with obesity and obesity increases with higher levels of insulin resistance. It is likely a vicious cycle, where the underlying genetic susceptibility or unhealthy diet leads to increased insulin levels and obesity, and the subsequent increasing obesity further perpetuates the insulin resistance and hyperinsulinemia.
- Pregnancy - Normal pregnancies, especially in the third trimester, show signs of insulin resistance. This is believed to be an evolutionary adaptation to preferentially provide glucose to the rapidly growing fetus. However, in susceptible individuals, this process can also lead to gestational diabetes and high blood pressure. This appears to be a good example of how a normal adaptive process designed to make us more successful in an initial hunter-gatherer environment can malfunction when exposed to the wrong environment, such as our modern diet full of foods high in refined carbohydrates and sugars.
- Metabolic syndrome - Insulin resistance is often used interchangeably with the term metabolic syndrome. While they are not technically the same, they do share similar characteristics, and both share the risk of progressing to type 2 diabetes. Metabolic syndrome is defined as three or more of the following markers: fasting blood glucose above 100mg/dL (5.5 mmol/L); elevated triglycerides above 150mg/dL; High Density Lipoproteins (HDL) below 40mg/dL in men and 50 in women; elevated blood pressure above 130/85; and increased abdominal obesity with a waist circumference over 40 inches in men and 35 inches in women. All of these characteristics tend to be common in insulin resistance as well.
- Pre-diabetes - Insulin resistance is associated with pre-diabetes, which is defined as fasting blood glucose of 100-125mg/dl (5.5 to 6.9 mmol/L), or an HbA1c of 5.7% or above. Since a pre-diabetes diagnosis depends on an elevated blood glucose level, it implies that insulin levels have been chronically elevated preceding the diagnosis.
- Polycystic ovary syndrome (PCOS) - Polycystic ovary syndrome (PCOS) is a common metabolic disorder affecting up to 10% of women of childbearing age. It's a leading cause of infertility, and a significant risk factor for future type 2 diabetes. Women with PCOS tend to have elevated levels of male hormones, irregular or absent menstrual periods, and/or cysts on their ovaries. Other common symptoms are obesity, acne, male-pattern hair loss, and excess facial and body hair. A common feature in both obese and lean women with PCOS is insulin resistance.
- Non-Alcoholic Fatty Liver Disease - Called NAFLD, this condition is marked by the accumulation of too much fat in the liver. While it is more common in individuals who are obese, who have metabolic syndrome, or who have type 2 diabetes, it has been found to be associated with insulin resistance and hyperinsulinemia in lean individuals with normal glucose tolerance. While not all people with NAFLD go on to develop liver problems, in some instances the condition leads to liver inflammation, scarring, and potential cirrhosis and liver failure.
- Cancer - Insulin resistance is associated with an increase in cancer-related growth factors and a greater risk of certain cancers. In particular, insulin resistance is associated with colorectal cancer, endometrial cancer, pancreatic cancer, and breast cancer. It is not clear yet, however, whether it is the insulin resistance itself or its relationship to other risk factors, such as obesity and high blood sugar, that contributes to the increased cancer risk. However, mechanistic data suggests chronically high levels of insulin may promote cancer growth and that restricting insulin may slow cancer growth.
- Cardiovascular disease (CVD) - Insulin resistance and hyperinsulinemia are associated with increased risks for cardiovascular disease, in part because it is so closely associated with other CVD risk factors such as obesity and hypertension. Some studies suggest, however, that insulin resistance is an independent risk factor for heart disease. Many mechanisms are proposed by which hyperinsulinemia triggers progressive heart disease. Most of them center around increased chronic inflammation and oxidation as well as direct vascular damage.
- Alzheimer's disease - Recent evidence suggests that Alzheimer's disease, now sometimes called type 3 diabetes, could also be linked to insulin resistance. Studies show that those with diabetes are 60% more likely to develop dementia. Another study shows an increased prevalence of brain tangles in those with diabetes. Although the exact mechanism is not proven, the theory is brain cells become insulin resistant and then cannot use glucose efficiently for fuel, thus leaving the cells starving for energy. The result is eventual progression to Alzheimer's disease.
- Adaptive insulin resistance - Eating very-low-carb diets has been associated with a condition called adaptive insulin resistance (also sometimes called physiologic insulin resistance or adaptive glucose sparing.) The mechanics of this phenomenon are debated, but the main hypothesis is that if we stop eating sugar or carbohydrates, the amount of glucose in our blood will fall. Our body will make sure, however, that our brain gets the glucose it needs by not taking up as much glucose in the liver, fat cells and muscle cells (thus those cells become "insulin resistant"). Those muscle and liver cells now use ketones as the preferred fuel source and regulate their insulin sensitivity without an increase in the overall glucose and insulin levels, both of which remain low. Since this type of insulin resistance occurs with low rather than high levels of circulating insulin, it is not felt to represent the same dangerous condition as regular insulin resistance and may actually be a good thing.
Diagnosing insulin resistance
How do you know if you have insulin resistance? What tests can you have that will confirm the diagnosis?
Unfortunately, insulin resistance is rarely diagnosed in most medical practices. It's not because it isn't widely prevalent in society, but because doctors don't generally order the tests for it. In addition, tests for insulin levels are expensive and not available in all locations.
Doctors more often order the standard tests for diabetes: fasting blood glucose and hemoglobin A1c. But these don't show a problem until the blood glucose has become too high, by which time insulin levels have likely been high for years if not decades.
What can you test if you don't want to wait until pre-diabetes or type 2 diabetes develops?
That's simple: measure your waist and your height!
Waist-to-height: a powerful predictive measure
One of the earliest symptoms of insulin resistance is an expanding waistline as the body stores fat in your abdomen.
Even people with "healthy" body mass index numbers between 20 and 25, can have fat collect in their abdomens if they are becoming insulin resistant. This situation is sometimes called TOFI - thin on the outside, fat on the inside. The fat is literally wrapping itself around the liver, heart, kidneys, pancreas and other organs.
That's why the size of your waist in relation to your height will tell you a great deal about your insulin sensitivity. Greater abdominal circumference in relation to height is related to an increased risk of diabetes, hypertension, cardiovascular disease and overall mortality even in people of normal weight. While this isn't a perfect test, it is very easy to do, does not require your doctor to order it, and it can give you a good starting point to see if you have insulin resistance.
To get your ratios you just divide your waist measurement by your height. A waist-to-height ratio less than 0.5 indicates good insulin sensitivity, while a number higher than 0.5 indicates worsening insulin resistance.
You don't even need a tape measure. Just take a piece of string! The length of string around your waist should be at most half your height. If your waist is larger than half your height, you likely have insulin resistance.
One of the great strengths of this measurement is that it doesn't matter what your ethnicity, whether you are male or female, young or old, short or tall, muscular or wiry: a number higher than 0.5 indicates an increased risk.
Many health campaigns are now encouraging this simple idea: "keep your waist to less than half your height."
Chart your waist and height
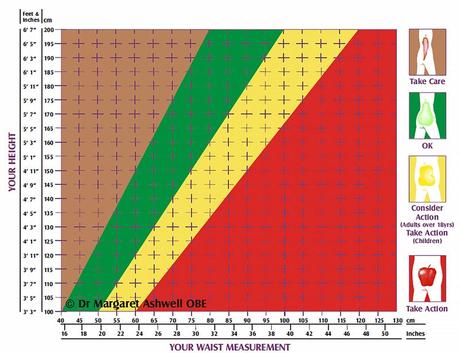
UK researcher Dr. Margaret Ashwell has pioneered the use of the Ashwell Shape Chart, which shows colored zones for waist-to-height measurements.
This simple graph can show you the danger zones. Just chart your waist measurement against your height and you can see where you fall in the graph.
Working with your doctor
As noted, most doctors don't routinely test for insulin resistance. They wait instead for pre-diabetes or type 2 diabetes to develop.
However, armed with the results of your waist-to-height ratio, if it is larger than 0.50, you can talk with your doctor about ordering follow up tests to confirm that insulin resistance is present, and that you are at risk for blood sugar and metabolic problems.
You will likely have to ask for these tests. Don't be afraid to be proactive and educate your doctor about these tests if you request them, as they are well worth the effort.
The top two tests we recommend are:
- Fasting insulin and fasting triglycerides. With this test, a blood test is taken first thing in the morning before you have eaten. Your insulin levels and your triglyceride levels are then measured. Triglycerides are a routine test that are easy to do, but fasting insulin, on the other hand, is less commonly ordered and you will likely have to ask for it specifically. One study showed these labs had the strongest association with insulin resistance. Since fasting insulin by itself is only really helpful if very high (>20) or very low (<3), combining a mildly elevated insulin with elevated triglycerides (>150) enhances the sensitivity, making insulin resistance much more likely.
- HOMA-IR- Homeostatic Model Assessment for Insulin Resistance. This is a fancy name for a simple test of both your fasting blood glucose and fasting insulin levels. It takes those two results and plugs them into a special calculator and gives you a numeric result. The concept is simple: How high does your insulin need to be to maintain your fasting glucose level? As an example, a fasting glucose of 95 mg/dL (5.3 mmol/L) with an insulin of 3 gets the HOMA-IR number of 0.7, suggesting good insulin sensitivity. But that same fasting glucose with an insulin level of 27 gets the HOMA-IR number of 6.3, suggesting clear insulin resistance and hyperinsulinemia. Any HOMA-IR number under 1 suggests good insulin sensitivity, while over 1.9 indicates early insulin resistance and anything over 2.9 indicates significant insulin resistance.
Summary
Awareness of and testing for insulin resistance, even with a simple waist-to-height measurement, should be more common among doctors and patients. If we wait for a rise in blood glucose, then we have missed years of high insulin levels that could have been reversed.
Instead, we want to identify insulin resistance early so we can reverse it and prevent the dangerous consequences of metabolic disease.
If you have confirmed insulin resistance, a number of proven lifestyle changes can be very effective to reverse the condition, including a low-carb, ketogenic diet, exercise, sleep, stress reduction and tobacco cessation. Check out our in-depth insulin resistance treatment guide for more detailed information.
Diet Doctor - How to treat insulin resistance
/ Dr. Bret Scher, MD

