Much new and interesting data support the benefits of fasting in diseases other than obesity and type 2 diabetes. This often relates to the role of nutrient sensors in the body. Everybody always believes that increased growth is good. But the simple truth is that excessive growth in adults is almost always bad.
Excessive growth is the hallmark of cancer, for example. Excessive growth leads to increased scarring and fibrosis. Excessive growth of cysts leads to the disease of polycystic kidney disease (PCKD) and polycystic ovarian syndrome (PCOS). Excessive growth in adults tends to be horizontal, not vertical. In most cases of adult disease, we want less growth, not more.
This leads naturally to the topic of mechanisms where the body regulates growth. One of the most exciting areas of research focus around nutrient sensors. Insulin is one example of a nutrient sensor. You eat protein or carbohydrates, and insulin goes up. This signals the body that there are enough nutrients to increase growth. Insulin is well known as a growth factor as well and shares a lot of homology with IGF-1 - Insulin Like Growth Factor.
Insulin has long been linked to cancer. Patients with insulin resistance and obesity, conditions characterized by high insulin levels are at high risk of all sorts of common cancers such as lung and colorectal. Diabetics who take insulin compared to those on oral medications almost double their risk of cancer. We will cover these topics in more detail sometime in the future.
But there are other nutrient sensors as well. mTOR is mammalian (or mechanistic) Target of Rapamycin. It was discovered when researchers were looking for the mechanism of action of a novel immune suppressing drug called rapamycin. It enjoys widespread usage in transplantation medicine. Because most anti-rejection medications suppress the immune system, there is an increased risk of cancer. What was unusual about this particular drug was that it decreased, rather than increased risk of cancer. It turns out that mTOR is also a nutrient sensor.

mTOR is mostly sensitive to proteins and certain amino acids. When you eat no protein, mTOR activity is decreased. With rapamycin, you could block mTOR with a drug and this would decrease cellular growth and thus impair certain types of cancer.
A third type of nutrient sensor are the family of proteins known as the sirtuins. Sirtuins were first isolated in 1999 in yeast and SIR stood for Silent Information Regulator. SIRs were subsequently isolated in everything from bacteria to humans and, like mTOR are a group of proteins conserved largely throughout all lifeforms. Interestingly, these proteins directly link cellular metabolic signaling to protein manufacturing.
SIR was first known to be involved in aging when genetic screens of long lived yeast found mutations in the SIR2 gene. Deletion of this gene shortened lifespan where overexpression increased it. In mammals, there are 7 sirtuins SIRT1 to SIRT7 and the most studied is SIRT1. When insulin is blocked, SIRT1 is shuttled out of the nucleus of cells into the cytoplasm, increasing levels (lower insulin = higher SIR1 = good). There is increasing evidence that SIRT1 is profoundly involved in cancer, apoptosis, and neurodegenerative diseases. The effects of SIRT1 on cancer are controversial. The pro-survival effects of SIRT1 may promote cancers, but on the other hand, it also clearly functions as a tumor suppressor. SIRT1 helps with DNA damage repair and thus may reduce cancer rates.
Polycystic kidney disease
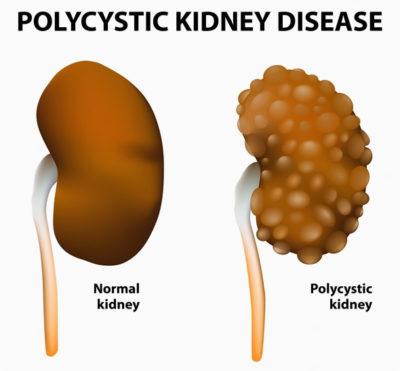
These patients develop thousands of cysts in the kidney and liver, which eventually destroys the functional tissue. When the kidneys are destroyed, the patients go into renal failure and require dialysis. Since patients have this from birth, it often takes 50-60 years of this disease to destroy kidney function. Interestingly, it is hypothesized that PCKD cells may also develop metabolic adaptations compatible with an increase in glycolytic activity similar to cancer cells.
The mTOR kinase is thought to play a key role in progression of the growth of these cysts. In mice, supplementation of the diet with branched chain amino acids, specifically leucine (which activate mTOR) significantly increased cyst formation. The authors suggested that "BCAA accelerated disease progression by mTOR and MAPK/ERK pathways. Hence, BCAA may be harmful to patients with ADPKD".
Everolimus, a drug that blocks mTOR was shown in animal models to be able to delay the growth of these cysts. This drug was tested in PCKD patients in a randomized study published in 2010 in the New England Journal of Medicine. While the drug was able to slow the growth of cysts, it was unable to slow the progression of kidney failure, and mTOR inhibitors are generally not used in the treatment of this disease. These drugs are largely considered a failure in the treatment of PCKD.
However, it does illustrate a very important point. In diseases of uncontrolled growth, the blockage of one of the nutrient sensors is able to slow down this unwanted growth. But what is generally unrecognized is that it simply makes no sense to shut down only one of at least 3 different nutrient sensors. Blocking mTOR pharmacologically does nothing to bring down insulin or increase SIRT1. It turns out that Sirtuins play a role in kidney health, although the effects are still largely investigational.
This therefore brings up an interesting possibility. Rather than trying to block nutrient sensors, why not simply restrict all nutrients, thereby naturally lowering the stimulus to the sensors. This would simultaneously lower insulin and mTOR while raising SIRT1. Wouldn't it be far more effective to work on all the nutrient sensors to decrease growth, rather than one at a time? What about using therapeutic fasting for the treatment of PCKD? This should be a far more powerful strategy for reducing unwanted growth.
Animal studies show that this could be done successfully. In mice, they use severe caloric restriction reducing intake by 30-50%. Sure enough, the kidney cyst growth was inhibited. While the applicability to humans is unknown and precise molecular mechanisms are unknown, it nevertheless suggests a tantalizing therapeutic strategy for PCKD, but also more broadly to all disease of excessive growth (cancer). Why not simply fast, signalling to the nutrient sensors that no food is available? This will then signal the body to slow down unneeded growth (cyst cells and cancer cells). This treatment is free and available to everybody.
Polycystic ovarian syndrome
The same exciting possibility exists for PCOS. It is well known that PCOS is intimately connected to insulin resistance. As I've argued many times, hyperinsulinemia and insulin resistance are just one and the same disease. High insulin levels will encourage growth of cells. These are diseases of excessive growth, in which insulin, as a nutrient sensor is making it worse. In females of reproductive age, the most rapidly growing cells are the ovaries, so the hormonal environment is encouraging excessive growth of these cysts in the ovaries. With fasting, or any other weight loss, like LCHF diets, for example, decreasing the insulin helps weight loss, but also reverses the PCOS in many cases.
Hyperinsulinemia appears to increase the effect of luteinizing hormone (LH) to increase androgen production (testosterone) which produces many of the clinical effects of PCOS. In addition, insulin decreases Sex Hormone Binding Globulin (SHBG) which increases the amount of free testosterone in the blood which increases the masculinizing symptoms (hair growth etc.) seen in PCOS. While this is an interesting hypothesis, little data exist to show whether this approach will work. However, given the low risk of skipping a few meals here and there, it seems reasonable to give this a try.

