If you've ever had an attack of diverticulitis, which is due to inflammation or infection of a small pouch in the wall of the lower intestine, you'll likely never forget it.
Intense, sharp pain, usually on the lower left side of your abdomen, likely had you doubled-over in agony. The pain may have also radiated across your lower abdomen, to your belly button, or possibly into your back or side.
If your attack was severe, possibly due to a perforation (hole) in your intestinal lining, you may have been hospitalized for treatment or required emergency surgery.
Clearly, you'll want to do whatever you can to avoid another attack.
Start your FREE 30-day trial!
Get instant access to healthy low-carb and keto meal plans, fast and easy recipes, weight loss advice from medical experts, and so much more. A healthier life starts now with your free trial!
Questions about low carb
If you've had diverticular disease and you're considering the low-carb or keto diet for weight loss, diabetes reversal, or other health reasons, you may have questions:
- Can you safely do a low-carb or keto diet with a history of diverticulitis?
- Could a low-carb or keto diet potentially put you at a higher risk of another diverticulitis attack?
- Or, could a low-carb or keto diet possibly help prevent a future attack?
This evidence-based guide will help answer these questions. It will explain what is known and not known about diverticulitis and highlight risk factors that can spur the condition.
The guide will also discuss the current research on which foods to eat or to avoid to prevent a recurrence of diverticulitis and during an acute diverticulitis attack.
What we know, and what we don't
Let's be upfront about one key point: in regards to the low-carb or keto diet, no high-quality studies have examined diverticulitis and this way of eating. Well-designed randomized controlled studies are sorely needed.
However, to help bridge the current knowledge gap, the creation of this guide included consulting Diet Doctor's international panel of medical experts and the international gastroenterologists listed on our Find a Doctor map of low-carb physicians.
These low-carb medical experts' consensus is that a person with a history of diverticular disease can safely eat a low-carb or keto diet without increasing their risk of a recurrence of this serious, painful condition.
In fact, in their clinical experience, by helping reduce obesity, metabolic syndrome, and chronic inflammation and removing refined carbohydrates and sugar from the diet, the low-carb, keto diet likely helps patients reduce their risk factors for an initial attack or recurrence.
As a U.S. gastroenterologist and the author of this guide, I agree with this clinical opinion. I routinely recommend the low-carb diet to virtually all my patients with gastrointestinal issues. In my clinical practice and through my research, I have no hesitation in recommending the low-carb or keto diet for anyone with diverticular disease.
However, in the absence of definitive high-quality research evidence, you must be comfortable making a decision that is right for you. Read on for a more in-depth discussion of these complex issues around a common health condition.
What is diverticulitis?
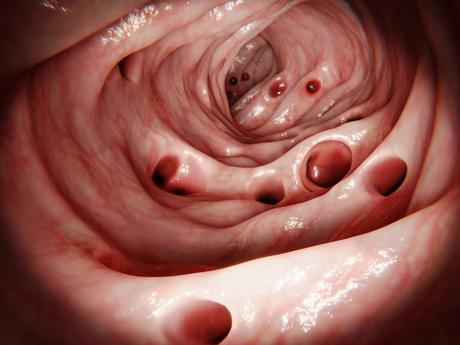
Diverticulitis occurs when small pockets or pouches in the lining of the intestine become inflamed or infected. They can even perforate or rupture with subsequent leakage of intestinal contents into surrounding tissue in more complicated cases.
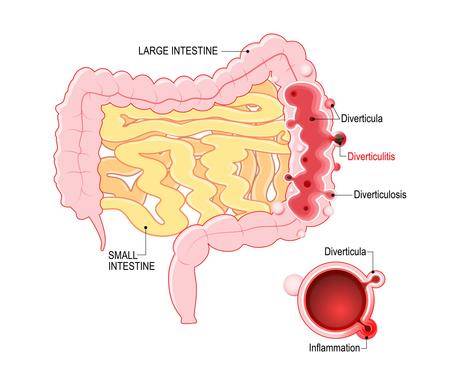
These pockets are called diverticula; a single one is called a diverticulum. They look like small potholes along the lining of the colon's inner wall. The condition of having diverticula is called diverticulosis and usually causes no symptoms.
Why do diverticula occur in the first place? That's not clear. It's thought to be a mixture of aging and heredity, combined with other triggers, such as smoking, diet, or inflammation.
Takeaway
Diverticula are pockets or pouches found in the lining of the large intestine.
With diverticulosis, these pockets usually cause no problems or symptoms, but, in a small percentage of people, the pockets may become inflamed or infected, called diverticulitis. In complicated cases of diverticulitis, the pockets may even perforate, leading to serious complications.
How common is it?
Diverticular disease is common in Westernized countries. In fact, for the last century, it has been deemed a disease of Western civilization.
Rates of diverticular disease increase as individuals migrate to developed nations or whole countries adopt a more western lifestyle. The incidence of diverticular disease is now increasing in other parts of the world, like Africa and Asia, where it used to be very rare.
Due to the large increase in screening colonoscopies over the last few decades, diverticulosis is now one of the most common incidental findings.
Recent studies have found that only about 4% of those with diverticulosis will develop diverticulitis.
Nevertheless, because diverticulosis is so common, millions of people in western countries experience a debilitating attack of diverticulitis each year. In the US alone, diverticulitis is the reason for more than 2.7 million outpatient visits and 200,000 hospitalizations annually.
Another concerning trend is that the incidence of diverticulitis is increasing, especially among those under the age of 50, in whom it used to be very rare. This increase at younger ages is worrisome. That's because the younger you are when diverticulosis is diagnosed, the higher your risk of eventually developing an attack of diverticulitis and then having recurring attacks.
Takeaway
Diverticular disease is common in all westernized countries, especially with advancing age. However, fewer than 5% of people with diverticula will go on to have attacks of diverticulitis. In recent years the incidence of diverticulitis has been increasing, especially in people under age 50.
Risk factors for diverticular disease

Since diverticula are so common and often arise without symptoms or issues, what are the other key risk factors, besides age, for their creation and for developing diverticulitis?
Here is the research evidence to date:
- Obesity: Obesity and excessive weight gain in adulthood increase the risk of diverticulosis, as well as the progression to diverticulitis. Those who are obese have more severe complications if diverticulitis arises.
It is theorized, although not proven, that the risk may be more due to changes in the microbiome of the intestine, likely from eating highly processed sugar and starches.
Takeaway
Several risk factors are associated with higher rates of diverticular disease, including advancing age, genetics, smoking, obesity, inactivity, diabetes, inflammation, altered microbiome, and perhaps a vitamin D deficiency. Dietary factors are assumed to be a risk, but results are inconsistent.
Foods to eat or avoid
What food should you eat to prevent diverticular disease? What foods should you avoid?
The role of specific food groups as factors in both causing and preventing diverticular disease has been a focus of study for decades. However, the research is still highly controversial and full of conflicting results.
Here is what current research says about specific foods:
Fiber
For decades it was thought that not eating enough fiber in the diet, and the resulting constipation, caused diverticulosis and increased the risk of diverticulitis. However, as one prominent researcher has recently noted, the fiber deficiency hypothesis "existed for four decades without any proof."
Over the last decade, some studies have found that eating more fiber does not prevent diverticula from forming.
Likewise, a few recent studies have also shown that, counter to the medical dogma for 50 years, constipation seems to have little or no relation to diverticular disease.
In fact, some studies are now suggesting that higher fiber diets, and more frequent bowel movements, may be more likely to be associated with the creation of diverticula.
However, here's where it gets more complicated. While high-fiber diets may not prevent diverticula from forming, observational data suggest that a high-fiber diet may reduce the risk of an acute attack of diverticulitis and may prevent more serious complications.
Whether an increase in fiber increases the risk of developing diverticulosis but reduces the likelihood of developing diverticulitis will require further study. The conflicting results may also be related to the type of fiber that is consumed, such as whether a fiber is soluble or insoluble, or from fruit and vegetables rather than cereal grains or bran.
However, eating a high-fiber diet seems to be good for general health, independent of diverticular disease. For a greater understanding about various types of fiber and how to get more low-carb fiber in your diet, please see Diet Doctor's evidence-based guide: 15 high-fiber foods that are low in carbs.
Nuts, seeds, and popcorn

For decades, both the medical profession and the general public believed that if you have diverticulosis or diverticulitis, you should avoid eating nuts, seeds, and popcorn.
It was thought these hard, undigested bits of food were more likely to get caught in the diverticular pouches or scratch or irritate them, leading to inflammation and infection.
However, the advice to avoid foods like popcorn, raspberries, strawberries, blackberries, and nuts was based on a logical assumption and lacked scientific evidence. In 2008, a large prospective study, which followed more than 47,000 men over 18 years, found no relationship between eating nuts, seeds, and popcorn and the incidence of diverticulitis. In fact, men who ate the most nuts and popcorn had less diverticulitis than men who ate the least.
Meat
Observational data show that eating large amounts of unprocessed red meat is associated with an increased incidence of diverticulitis in men.
However, like many studies about meat consumption in recent years, in this study, men with the highest consumption of red meat also tended to smoke more, used NSAIDs more, and were less likely to exercise than the men with the lowest meat consumption. This is called the healthy user bias.
As well, the study suffers from the many other methodological flaws of observational nutrition studies, including that the relative risk difference between the highest level of meat-eaters and the lowest was very small.
The Diet Doctor evidence-based guide on red meat goes into more detail about the poor quality, observational evidence that makes it very difficult to make any strong conclusions about the impact of red meat consumption on various health conditions.
"Healthy" or "prudent" diet - or no special diet at all?
Some researchers advise that to reduce your risk of diverticulitis, eat a "healthy," non-Western or "prudent" diet. What does that mean? The researchers describe the "Western" dietary pattern as one with a high intake of red and processed meats, refined grains, sweets, French fries, and high-fat dairy products. A "prudent diet" was described as high in fruits, vegetables, whole grains, legumes, poultry, and fish.
What part of the prudent diet actually decreases the risk? Could it be that eliminating refined grains and sweets is the essential part of decreasing the risks of diverticulitis? This research question has not been explored.
One small but influential study found that during an attack of uncomplicated (or less severe) diverticulitis, it didn't really matter what people ate, that an unrestricted or liberal diet had the same outcomes as those who restricted certain foods. This finding, along with the other conflicting dietary studies, has led many doctors and dietitians to no longer recommend specific diets.
Nevertheless, many people with recurrent diverticulitis find that some specific foods tend to precede their attacks and learn to recognize and avoid their personal triggers. Paying attention to your possible dietary triggers may help you manage your diverticular disease.
Takeaway
The role of a high-fiber diet in diverticulosis and diverticulitis is now questioned and complicated by weak associational data.
Nuts, seeds, and popcorn do not seem to be associated with attacks.
The general advice is to eat a "healthy" or "prudent diet" but specific restricted diets may not be necessary and individuals should find the diet that is right for them.
Low-carb, ketogenic diet

Many people come to the low-carb or keto diet for help with obesity and diabetes. Since these conditions are also underlying risk factors for diverticulosis, it is only natural that many considering the low-carb diet may be worried whether they can safely do the diet without aggravating their diverticulitis.
As noted in the opening of this guide, currently no high-quality trial has been conducted comparing a low-carb or ketogenic diet to other dietary patterns among those who have diverticular disease.
Diet Doctor's expert panel and gastroenterologists who recommend low-carb diets on our Find a Doctor page were consulted. The consensus is that in their clinical experience the diet is safe for those with diverticular disease.
They make the following observations as to why they recommend low carb to patients with diverticular disease:
- The unexplored role of sugar and refined carbohydrates in diverticular disease: As a disease of Western civilization, diverticulitis has increased in parallel with the consumption of sugar and refined carbohydrates since the 1860s. In fact, a highly influential research paper in 1971 hypothesized that diets high in sugar and refined carbohydrates could be the key underlying risk factors for the development of diverticular disease. However, this observation about the role of sugar and refined carbohydrates was ignored in favor of holding low-fiber diets responsible for diverticular disease for the next 50 years.
To date, no research has been carried out on any possible links between high consumption of sugar, refined carbohydrates and processed food. We believe these food groups should be studied, given the risk factors of obesity, diabetes, and chronic inflammation underlying diverticular disease.
Anecdotally, many people eating a low-carb or ketogenic diet report an improvement in other inflammation and gastrointestinal symptoms, including a reduction in irritable bowel syndrome (IBS), heartburn (gastric reflux), and inflammatory bowel disease.
Our guide IBS and the keto diet provides more in-depth discussion around the research and clinical experience for this other common intestinal condition.
Diet Doctor has success stories from Ruth and Jennifer about how they feel they greatly improved their symptoms of diverticular disease by eating a ketogenic diet.
Takeaway
Studies show that obesity, diabetes, metabolic syndrome, and markers of chronic inflammation respond well to a low-carb, ketogenic diet. Since these are risk factors for diverticular disease, reducing them may help decrease the risk of diverticulitis. Plus, anecdotal evidence is increasing that symptoms and flares of diverticular disease may be reduced by low-carb eating. But scientific studies showing this are lacking.
Intermittent fasting
During an attack of diverticulitis, the medical recommendation is that patients should only consume clear fluids for two or three days or until their symptoms improve. If the attack is more severe (called complicated diverticulitis), the recommendation is to take nothing by mouth until the diverticulitis heals. This is a therapeutic form of intermittent fasting to heal the gut.
A clear fluids diet means consuming water, sparkling water, mineral water, unsweetened tea, black coffee, consommé, and bone broth. Some doctors allow sweetened clear juice, jello, sugary drinks, or diet drinks with artificial sweeteners, but low-carb doctors, like myself and others on the Diet Doctor expert panel, recommend avoiding all fluids with sugar and artificial sweeteners.
My clinical advice is that if you are doing the low-carb diet and happen to have a flare of diverticulitis, you may want to fast for a few days, drinking only clear beverages. But when you feel better, you can go right back to the low-carb diet.
Could adopting intermittent fasting in times other than acute attacks help prevent or reduce flares of diverticular disease?
Unfortunately, no research studies have been conducted on the possible role of regular episodes of intermittent fasting on diverticular disease. Good studies are needed. However, a logical argument can be made that periods of fasting could be beneficial to the underlying intestinal pathology of diverticular disease.
A short pattern of intermittent fasting, such as skipping breakfast or eating one meal a day ( OMAD) is unlikely to be harmful for someone with diverticular disease and can help with weight loss, diabetes, and blood sugar management.
For more information about intermittent fasting, see Diet Doctor's guides and videos.
Takeaway
A clear liquid fast for two or three days is recommended for treating acute diverticulitis.
Research is lacking for the regular use of intermittent fasting to prevent flares of diverticular disease, but intermittent fasting is effective for underlying risk factors such as obesity and diabetes.
The clinical opinion of low-carb experts is that fasting is safe and may even be beneficial for diverticular disease.
Summary
Diverticular disease is common among the populations of all Westernized countries, particularly as people age. Obesity, diabetes, smoking, inactivity, and chronic inflammation are all risk factors.
A high-fiber diet likely does not prevent the development of diverticular disease, but it may reduce complications and hospitalizations from acute attacks.
Doctors and dietitians no longer recommend specific restricted diets for diverticular disease, and so you are encouraged to find a diet that works best for you and makes you feel your healthiest. For many people, this may be a low-carb or ketogenic diet.
No research evidence is not yet available to make conclusions about a low-carb diet, keto diet, or intermittent fasting, in relation to diverticular disease. However, clinical experience, and some patient testimonies suggest that both the diet and periodic fasting is not only safe but could be beneficial for the health of the entire digestive tract.

