A new study published last week has the autism community asking new questions about early diagnosis and prediction. A publication in Molecular Psychiatry has been titled by the media as “Researchers Claim 100% Accuracy Predicting Autism Risk Factors in Mom’s Blood”. Disappointingly, one of my favorite sites called IFLS (or I f**king love science) titled it “Algorithm Predicts A Type of Autism With 100% Accuracy Using Mother’s Biomarkers”. Why am I disappointed in IFLS and other headlines? Because I don’t think families should interpet or utilize these findings as an established and validated method of predicting autism in their children or potential children. In their defense, the researchers did not title the study in this way, that was the media’s interpretation.
This is a story that goes back a decade. In 2007 researchers at UC Davis had identified specific antibodies in mother’s blood that were associated with an increased probability of having a child with autism. The idea was that an antibody in mother’s blood reacted to the developing brain of their fetus, leading to brain abnormalities associated with a greater likelihood of an autism diagnosis. It started with a class of antibodies, then narrowed down to different general sizes of antibodies, and more recently these antibodies were given names. The theory has been tested in different ways. Animal models have shown that exposure to these antibodies leads to changes in brain cells in areas that are consistent with autism behaviors. Children with ASD born from mothers who have these antibodies have been shown to have enlarged head size. The work has mainly been done at UC Davis, but other groups have also been investigating the link.
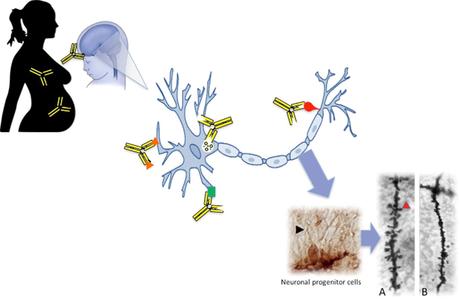
From Jones and Van deWater, 2018. This depicts the maternal autoantibody transmission to the brain, which then affects the size and shape of neurons of the child with ASD.
Of course, it isn’t an all or nothing thing. The UC Davis group estimated a whopping 23% of mothers with children with a diagnosis had autoantibodies were present, other researchers studying the question put it at 8-10%. Regardless of the exact number, this is an increased rate of diagnosis compared to about 1% in the general population. As a result, researchers in the UC Davis group set up a commercial entity called Pediatric Biosciences, which has since folded, to produce a test that would identify these proteins in mother’s blood so they could be aware of an increased risk of an autism diagnosis. The goal has been to identify a group of women who have a heightened probability of having a child with ASD so that that information can be conveyed to them in future family planning decisions.
This recent study that calculated the 100% specificity number used machine learning, which is an algorithm developed and run through a computer, to identify which combination of 7 of these autoantibodies were the ones that led to the diagnosis in the child, since presence of just one was insufficient. For example, if the mother has autoantibodies to something called CRIMP1 and GDA, there was a 100% probability that the child would have an autism diagnosis. This is interesting, right?
Well, there are reasons to temper your enthusiasm right now and don’t run out and get this maternal autoantibody test or rely on it. First, the sample sizes were kind of small to make the claim that it had “100% specificity”. Yes, maybe in these studies, small groups of people with ASD (groups with 20 children or less) also had mothers with a combination of the 2 antibodies (compared to none or very few in the controls), but it needs further comparison and the acknowledgement that there are many more children born to mothers without this antibody who also have an ASD diagnosis, and there are other factors that we also know to be involved in risk for ASD, such as genetic factors or other environmental or maternal and paternal factors. Second, and most importantly, the samples they used were what is known as “retrospective”. They took blood from mothers in a study for those who had already had at least one child with autism. The samples were taken years after the diagnosis so the link between the autoantibodies and the actual cause of ASD is not a straight line. The authors have said they are studying this in prospective samples, that is, women who have a child with autism and are pregnant with a 2nd or even 3rd. This way they will be able to investigate the presence of the autoantibodies at the same time as the pregnancy and monitor the outcome of the child. Some researchers have suggested that these autoantibodies reflect an ongoing immune process based on other risk factors like arthritis, gestational diabetes or other immune conditions. More research using population-based and prospective samples would provide better information as to whether or not these autoantibodies are causal or secondary, or if it represents a subgroup with distinct features.
This story is a great example of how science has narrowed down an early hypothesis to an actual working theory through years of laborious research. However, more work needs to be done, and if you have an immune condition or are concerned and have questions about an individual family and probability of having a child with ASD, talk to your doctor. There are a lot factors that influence probability of a diagnosis, and more importantly, lots of factors that play out in real life, like genetic interaction, which we need to learn a whole lot about. This algorithm did not take anything else into consideration, and when you are talking about family planning, you need to have all the information you can. On the other hand, this research is meaningful for other reasons besides predicting the probability of an ASD outcome. This furthers the idea that there are many ways to subgroup people with autism – both biological and behavioral – and finding those right combinations is really the holy grail of understanding ASD.
