“More than 50% of all medicines are prescribed, dispensed or sold inappropriately, and half of all patients fail to take medicines correctly.”
WHO Fact Sheet 2012
So why do half of all patients fail to take medicines correctly?
Issues of adherence are different depending on whether the condition in acute chronic. For example, it is extremely common for patients to fail to take the complete course of antibiotics for an acute infection, thereby predisposing to antibiotic resistance. For background on adherence in relation to chronic conditions, you can freely download the WHO publication ‘Adherence to Long-term Therapies’ (1.5Mb): (Open Access)
Here are the “Take-home messages” (reproduced from the report):
1. Poor adherence to treatment of chronic diseases is a worldwide problem of striking magnitude
Adherence to long-term therapy for chronic illnesses in developed countries averages 50%. In developing countries, the rates are even lower. It is undeniable that many patients experience difficulty in following treatment recommendations.
2. The impact of poor adherence grows as the burden of chronic disease grows worldwide
Noncommunicable diseases and mental disorders, human immunodeficiency virus/acquired immunodeficiency syndrome and tuberculosis, together represented 54% of the burden of all diseases worldwide
in 2001 and will exceed 65% worldwide in 2020.The poor are disproportionately affected. The consequences of poor adherence to long-term therapies are poor health outcomes and increased health care costs
3. Poor adherence to long-term therapies severely compromises the effectiveness of treatment making this a critical issue in population health both from the perspective of quality of life and of health economics. Interventions aimed at improving adherence would provide a significant positive return on investment through primary prevention (of risk factors) and secondary prevention of adverse health outcomes.
4. Improving adherence also enhances patients’ safety
Because most of the care needed for chronic conditions is based on patient self-management (usually requiring complex multi-therapies), use of medical technology for monitoring, and changes in the patient’s lifestyle, patients face several potentially life-threatening risks if not appropriately supported by the health system.
5. Adherence is an important modifier of health system effectiveness
Health outcomes cannot be accurately assessed if they are measured predominantly by resource utilization indicators and efficacy of interventions.The population health outcomes predicted by treatment efficacy data cannot be achieved unless adherence rates are used to inform planning and project evaluation.
6. “Increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatments”1
Studies consistently find significant cost-savings and increases in the effectiveness of health interventions that are attributable to low-cost interventions for improving adherence. Without a system that addresses the determinants of adherence, advances in biomedical technology will fail to realize their potential to reduce the burden of chronic illness. Access to medications is necessary but insufficient in itself for the successful treatment of disease.
7. Health systems must evolve to meet new challenges
In developed countries, the epidemiological shift in disease burden from acute to chronic diseases over the past 50 years has rendered acute care models of health service delivery inadequate to address the health needs of the population. In developing countries, this shift is occurring at a much faster rate.
8. Patients need to be supported, not blamed
Despite evidence to the contrary, there continues to be a tendency to focus on patient-related factors as the causes of problems with adherence, to the relative neglect of provider and health system-related determinants.These latter factors, which make up the health care environment in which patients receive care, have a major effect on adherence.
9. Adherence is simultaneously influenced by several factors
The ability of patients to follow treatment plans in an optimal manner is frequently compromised by more than one barrier, usually related to different aspects of the problem. These include: the social and economic factors, the health care team/system, the characteristics of the disease, disease therapies and patient-related factors. Solving the problems related to each of these factors is necessary if patients’ adherence to therapies is to be improved.
10. Patient-tailored interventions are required
There is no single intervention strategy, or package of strategies that has been shown to be effective across all patients, conditions and settings. Consequently, interventions that target adherence must be tailored to the particular illness-related demands experienced by the patient. To accomplish this, health systems and providers need to develop means of accurately assessing not only adherence, but also those factors that influence it.
11. Adherence is a dynamic process that needs to be followed up
Improving adherence requires a continuous and dynamic process. Recent research in the behavioural sciences has revealed that the patient population can be segmented according to level-of-readiness to follow health recommendations.The lack of a match between patient readiness and the practitioner’s attempts at intervention means that treatments are frequently prescribed to patients who are not ready to follow them. Health care providers should be able to assess the patient’s readiness to adhere, provide advice on how to do it, and follow up the patient’s progress at every contact. Health professionals need to be trained in adherence Health providers can have a significant impact by assessing risk of nonadherence and delivering interventions to optimize adherence. To make this practice a reality, practitioners must have access to specific training in adherence management, and the systems in which they work must design and support delivery systems that respect this objective. For empowering health professionals an “adherence counselling toolkit” adaptable to different socioeconomic settings is urgently needed. Such training needs to simultaneously address three topics: knowledge (information on adherence), thinking (the clinical decision-making process) and action (behavioural tools for health professionals).
12. Family, community and patients’ organizations: a key factor for success in improving adherence
For the effective provision of care for chronic conditions, it is necessary that the patient, the family and the community who support him or her all play an active role. Social support, i.e. informal or formal support received by patients from other members of their community, has been consistently reported as an important factor affecting health outcomes and behaviours.There is substantial evidence that peer support among patients can improve adherence to therapy while reducing the amount of time devoted by the health professionals to the care of chronic conditions. A multidisciplinary approach towards adherence is needed A stronger commitment to a multidisciplinary approach is needed to make progress in this area. This will require coordinated action from health professionals, researchers, health planners and policy-makers.
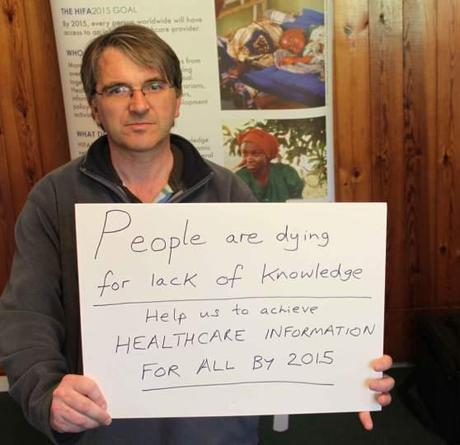
Author profile: Neil Pakenham-Walsh is the coordinator of the HIFA2015 campaign and co-director of the Global Healthcare Information Network. He is also currently chair of the Dgroups Foundation (www.dgroups.info), a partnership of 18 international development organisations promoting dialogue for international health and development. He started his career as a hospital doctor in the UK, and has clinical experience as an isolated health worker in rural Ecuador and Peru. For the last 20 years he has been committed to the global challenge of improving the availability and use of relevant, reliable healthcare information for health workers and citizens in low- and middle-income countries. He is particularly interested in the potential of inclusive, interdisciplinary communication platforms to help address global health and international development challenges. He has worked with the World Health Organization, the Wellcome Trust, Medicine Digest and INASP (International Network for the Availability of Scientific Publications). He is based near Oxford, UK.
He can he contacted at neil.pakenham-walsh AT ghi-net.org
Join HIFA2015 http://www.hifa2015.org
Editor’s Note: This is a guest post and the views expressed in the article are solely that of the author. The incidents about patient experiences stated in this blog(if any) are completely fictional and any resemblance to any person(living or dead)and/or incident is purely co-incidental.

