Disclaimer: This post reflects my personal opinion and does not represent any opinion or position of my employer (ICMR, GoI) or any agency I am affiliated with.
COVID-19 is a unique challenge, quite unlike any of the pandemics or epidemics we have experienced in recent times. Here's a rule of thumb calculation, which has rather chilling implications. If 100 at-risk persons are exposed to the virus, then, according to experts, and some modeling studies, 70 persons will contract the infection. Of these 70 people, 56 will have mild disease, many being mild to the point of being asymptomatic. Of the remaining 14 persons with moderate to severe disease, most will require hospitalization. Of those hospitalized, 3 persons will need some form of intensive care and ventilatory support will be needed in 1.5 people. Of these, about 1 person will die.
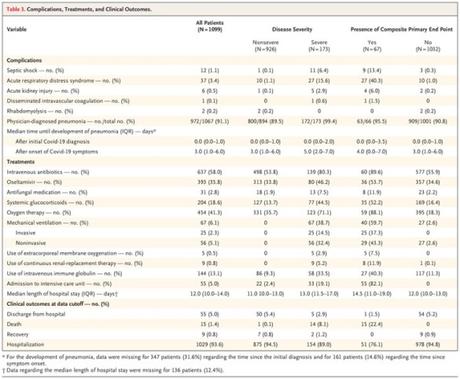
Now these are just back of the envelope calculations and are going to vary wildly based on the local contexts, but what remains clear is that there is going to be a massive demand for healthcare services in areas with intense transmission of COVID-19. For a better sense of these numbers, you can check out the original NEJM article which looks at the clinical features of 1099 patients and provides a pretty comprehensive picture.
There are two ways in which this challenge can be mitigated. Either staunch the number of cases arriving at the hospitals, by "flattening the curve", or scale up the available health service resources, so that the increased demands may be met.
According to the 2019 National Health Profile, in the government setup, India has 21,403 rural hospitals, with 265,275 beds, and 4,375 urban hospitals, with 448,711 beds. The Railways health systems has 122 hospitals, with 13,355 beds; and the ESI Corporation has 155 hospitals, with 21,931 beds. In addition, there are about as many beds in the private sector (perhaps even more). The World Bank estimates that India has a hospital bed density of 0.7 per 1,000 population. If the estimates in the NEJM paper are to be extrapolated, India is likely to land up with a deluge of patients requiring both hospital-based care and intensive care. Learning from the Italy experience, unless case loads are reduced, or spaced out over a longer period of time, it is very likely that the Indian health care system will be overwhelmed. Italy, which has 3.4 beds per 1,000 population - about 5 times as much as India's, has been overloaded to the point that health care workers and the health system is collapsing under the weight of the work load. The photo of a nurse, Elena Pagliarini, collapsed face down after a Herculean 10-hour shift, has become emblematic of the burden on Italy's healthcare workers.
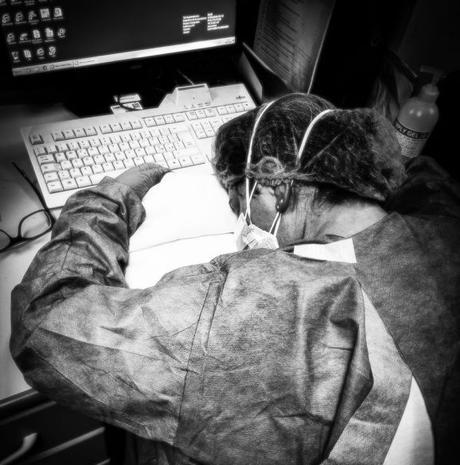
Elsewhere, in Spain, which has 3.0 beds per 1,000 population, according to the same World Bank data, another horrific tale has started to unfold. According to a New York Times report, the COVID-19 crisis has hit Spain with a double whammy: on one hand the toll of cases and deaths continue to rise exponentially; and on the other, scores of healthcare workers are contracting COVID-19 due to the constrains on resources, particularly the lack of protective PPEs. In fact, out of the 40,000-odd cases in Spain, there were 5,400 healthcare workers, representing a significant fraction of the healthcare work force. This toll has pushed the healthcare system to the "brink of collapse".
Given the limited resilience in the Indian healthcare system, and the worrying stories about the lack of PPEs, limited training for healthcare workers, and leaky lock down in place, it is extremely likely that we will not be able to manage the case loads if they reach Italy or US proportions. As bad as the general hospital bed density is, in India, the ICU bed density is even worse, standing at 2.3 beds per 100,000 population.
Hence, it becomes critical to reduce the case loads which reach the hospital. Ensuring community-facing interventions are successfully deployed and owned by the community members is perhaps the only way to ensure that we do not end up facing a challenge as large as the one in Italy or Spain. The fact remains that even now, with the global pandemic alert knocking on everyone's doors, people are still pooh-poohing the threat of COVID-19, as is exemplified by the continued mobility of people in and between Indian cities. Strategies will need to be framed, and then implemented, to ensure that the cases are limited to mild symptomatics who can be managed at home, using home-based isolation efforts. The more we rely on hospital-based care as a panacea for the COVID-19 threat in India, the steeper will be the gradient of mounting an adequate response.
We need to fight COVID-19 by limiting its spread in communities, while we still have a window of opportunity. It is very likely that community transmission is still not happening in India, and before the epidemic explodes, we need to nip its growth rate, otherwise, we shall lose the war against COVID-19, and our health care system, our health care workers will go down like ninepins.
