Anyone with an email account has received tips on how to augment their male anatomy. And while this might sound like content right out of such an email, it is, in fact, not so! A patient in South Africa received an allotransplanted penis, after he suffered tissue loss due to a botched traditional ritual circumcision which led to gangrene. In a case report published in The Lancet this week, the details of the patient’s follow-up over 24 months has been published. The course has been pretty unremarkable considering the novel solid organ transplantation and the likely complications that might have resulted. The abstract of the paper reads:
Methods
We first performed a cadaver-to-cadaver penile transplantation as preparation. After approval from the Human Research Ethics Committee was obtained, we recruited potential recipients. We screened the potential participants for both physical and psychological characteristics, including penile stump length, and emotional suitability for the procedure. A suitable donor became available and the penis was harvested. We surgically prepared the penile stump of the recipient and attached the penile graft. Immunosuppression treatment with antithymyocyte globulin, methylprednisolone, tacrolimus, mycophenolate mofetil, and prednisone were commenced. Tadalafil at 5 mg once per day was commenced after 1 week as penile rehabilitation and was continued for 3 months. We collected on quality-of-life scores (Short Form 36 version 2 [SF-36v2] questionnaires) before surgery and during follow-up and measured erectile function (International Index for Erectile Function [IIEF] score) and urine flow rates at 24 months post transplant.
Findings
The warm ischaemia time for the graft after removal was 4 min and the cold ischaemia time was 16 h. The surgery lasted 9 h. An arterial thrombus required urgent revision 8 h after the operation. On post operative day 6, an infected haematoma and an area of proximal skin necrosis were surgically treated. The recipient was discharged after 1 month and first reported satisfactory sexual intercourse 1 week later (despite advice to the contrary). The recipient reported regular sexual intercourse from 3 months after the operation. An episode of acute kidney injury at 7 months was reversed by reducing the tacrolimus dose to 14 mg twice per day. At 8 months after surgery, the patient had a skin infection with phaeohyphomycosis due to Alternaria alternata, which we treated with topical antifungal medication. Quality-of-life scores improved substantially after the operation (SF-36v2 mental health scores improved from 25 preoperatively, to 57 at 6 months and 46 at 24 months post transplant; physical health scores improved from 37 at baseline to 60 at 6 months and 59 at 24 months post-transplant). At 24 months, measured maximum urine flow rate (16·3 mL/s from a volume voided of 109 mL) and IIEF score (overall satisfaction score of 8 from a maximum of 10) were normal, showing normal voiding and erectile function, respectively.
Interpretation
Penile transplantation restored normal physiological functions in this transplant recipient without major complications in the first 24 months.
The surgical euphoria is literally tangible in this achievement, as it rightly should be. The approach of allotransplantation of the donor penis is a novel approach, which the group (led by Dr André van der Merwe) undertook in this patient, who had suffered penile loss three years ago. The conventional technique of reconstruction of lost penile tissue was the creation of a neophallus using flap of tissue from the forearm or lateral thighs. However, the complication rates for the process approached 40% in some case series and further, these were at a high risk of extrusion and urine leakage in a sexually active age group. Given the high costs of the procedure and the high proportion of patients suffering complications, the allotransplantation approach, therefore, represents a pathbreaking endeavor. Further, although apparently some sensation can be restored of the peripheral nerves are anastomosed well, the neophallus thus constructed has no inherent erectile activity, and thus need penile prostheses and other aids for undertaking regular penetrative intercourse. The high costs for the management of these procedures, all of which come at a cost, are virtually unmanageable in the context of resource limited settings. In comparison, the success of the process of allotransplantation is highlighted, once again, in the accompanying commentary:
By contrast with a patient having to wait an average of 1 year for a penile prosthesis to be implanted into a neophallus, the penile transplant recipient in this study experienced spontaneous natural erections 3 weeks after surgery and, despite medical advice to the contrary, had successful sexual intercourse at 5 weeks and was later able to impregnate his partner and have sexual intercourse without erectile aids by 6 months post transplant. Most importantly, the patient expressed early acceptance and sustained satisfaction with his transplanted penis, as shown by the near doubling of his mental health score to normal levels after receiving the transplant.
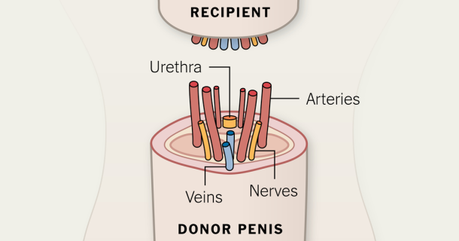
Penis Transplantation (Source: NY Times)
" data-orig-size="1050,550" sizes="(max-width: 610px) 100vw, 610px" data-image-title="nyt penis transplant imahe" data-orig-file="https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=610&h;=320" data-image-meta="{"aperture":"0","credit":"","camera":"","caption":"","created_timestamp":"0","copyright":"","focal_length":"0","iso":"0","shutter_speed":"0","title":"","orientation":"0"}" width="610" data-medium-file="https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=610&h;=320?w=300" data-permalink="https://scepticemia.com/2017/08/18/penile-transplantation-no-this-is-not-spam-mail-this-is-real/nyt-penis-transplant-imahe/#main" alt="Penis Transplantation (Source: NY Times)" height="320" srcset="https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=610&h;=320 610w, https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=150&h;=79 150w, https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=300&h;=157 300w, https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=768&h;=402 768w, https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=585&h;=306 585w, https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png 1050w" class="size-full wp-image-5368" data-large-file="https://scepticemia.files.wordpress.com/2017/08/nyt-penis-transplant-imahe.png?w=610&h;=320?w=585" />Penis Transplantation (Source: NY Times)
However, the public health physician in me, who has always worked in severely resource limited settings, feels ambivalent towards this kind of procedure. Ritual circumcision related gangrene and penile loss is, despite the sociocultural connotations, a preventable condition. Like many other cultural activities which are taboo and need to be cracked down upon (e.g. child marriage), this is a complex, yet detrimental cultural norm which needs to be reversed. If one is not brought up in a cultural setting where ritual circumcision is conducted, they are likely to wonder about the magnitude of the problem, and whether it merits such aggressive management options. However, an accompanying commentary in the same issue highlights the fact that infections and complications related to ritualistic circumcision are a fairly well recognized phenomenon, at least in the South African context:
Ritual circumcision is a rite of passage, during which the foreskin is removed, often by use of a non-sterile instrument such as a spear, and the men are sent into seclusion for 1 week thereafter. Complications are common and include infections, which result in hundreds of hospital admissions every year and tens of penile amputations and deaths.
Given that a solid organ transplantation is a complicated surgical maneuver, with high treatment and follow-up costs, how justified is it to undertake such a procedure for an entirely preventable malady? The authors have conducted a cost analysis, which I personally think under-estimates the overall expenses involved and they have come up with the following figures:
We did a cost analysis including surgical and anaesthetic services and the first month cost US$18653 while immunosuppression and clinic visits in the subsequent 2 months cost $1184 per month.
In an interview, Dr. van der Merwe admits that the costs for the forearm flap procedure can easily soar north of 120,000$ per case:
It’s very, very expensive. A forearm-flap penis costs about $120,000, and then an additional 10,000 to 12,000 U.S. dollars for one of those inflatable things. And then you tell the guy he can only have sex once in a week or once in two weeks because otherwise these things aren’t going to work? And then because you’re connecting different tissues, the flaps often leak urine, so men have to sit down to urinate. So, yes, it’s better than nothing but certainly it doesn’t have the same function as the real organ. Not by a far chance.
Keeping these numbers in comparison, the allotransplantation procedure seems like a great deal!
The patient is fortunate that the costs are being borne by the Western Cape Government, but given that these numbers are potentially affordable by a large section of the populace that might need the procedure, I think it deserves a closer and more detailed scrutiny to assess the actual costs – resulting from both direct and indirect causes.
I am not the only one to be raising this issue, and an article in the Journal of Medical Ethics (published by the BMJ Group) grapples with the same matter, at quite some length; to avoid redundancy I shall not mention the details of the article here again.
Finally, this line of ethical debate raises some interesting quandaries. Given the costs, the risks and the resource limited settings, is it legitimate for a person, who suffered penile loss due to a preventable accident/incident, like ritualistic circumcision, to claim a penile allotransplantation as a healthcare service that they should be entitled to? Would the situation be different for someone who is in the same medical boat, but due to entirely different sets of reasons – for example, they were hit by an IED while serving in the military, or they suffered the penile tissue loss in a gruesome road traffic accident not caused by their actions – would they be more eligible to receive this costly procedure? Given the fact that sexual activity has a “best by” age, would a seventy year old person, who is otherwise in perfect health, be eligible for receiving a penile transplant?
Sexual activities have multiple connotations and the impact of the procedure on the mental health aspect of the patient is clear as daylight. In the long term, innovation should not be muzzled by penny pinching and tightening pursestrings. The issue of penile allotransplantation, like any other organ transplantation, bears expenses and risks, and is topped off with an interesting set of biomedical ethics questions.
In any case, kudos to Dr. van der Merwe and his team, for this rousing success.
