In an experimental set up consisting of five different conditions - aerosol, plastic, stainless steel, copper and cardboard - it was observed that SARS-CoV-2 remained viable in aerosols over three hours, with a reduction in infectiousness titer from 10 3.5 to 10 2.7 TCID 50[1] per liter of air. The virus was more stable on stainless steel and plastic than on copper and cardboard, and viable virus could be isolated up to 72 hours post inoculation. However, virus concentration was greatly reduced in both cases: from 10 3.7 to 10 0.6 TCID 50 per milliliter of medium after 72 hours on plastic and from 10 3.7 to 10 0.6 TCID 50 per milliliter after 48 hours on stainless steel.[2] No viable virus could be isolated from copper surfaces after 4 hours and from cardboard after 24 hours. The virus showed exponential decay in titer over time. Median half-life of SARS-CoV-2 in different conditions were: 1.1 hours in aerosols; 5.6 hours on stainless steel; 6.8 hours on plastic; 0.8 hours on copper; 3.5 hours on cardboard.
WHO's situation report 32 further indicates that the virus may remain viable in a frozen state, existing up to 2 years at -20 deg C temperature. However, it notes that coronaviruses are thermolabile, hence, normal cooking conditions, where temperatures above 70 deg C are reached, may be adequate to inactivate the virus. The report further recommends that consumption of raw or undercooked animal-based food products should be avoided, and cross-contamination from such food materials with other raw or uncooked foods should also be guarded against.[3]
Computational fluid dynamics-based approaches have been used to also identify whether flushing a toilet can generate a turbulence strong enough to throw a plume of bioaerosols contaminated with the SARS-CoV-2 virus.[4] This is especially significant considering the finding that the virus may be excreted in the feces of as many as 67% of infected persons.[5]
Although these findings seem to suggest that viable virus may be isolated from surfaces from hours to days after contamination, they may not directly translate into infectiousness, as the viral titers reduce at a variable rate depending on the nature of the surface. However, the theoretical risk of contracting SARS-CoV-2 infection through fomite transmission remains possible. An outbreak investigation, linked to a mall in Wenzhou, China, hypothesized that the outbreak of COVID-19 in several patients who had no known contact with an index case, could have taken place through high touch surfaces, although it is possible that asymptomatic infected persons who were not detected in the mall could have been responsible for the spread of the virus.[6] The US CDC also states that fomite transmission, although possible, is not the principal route of spread for the virus.[7]
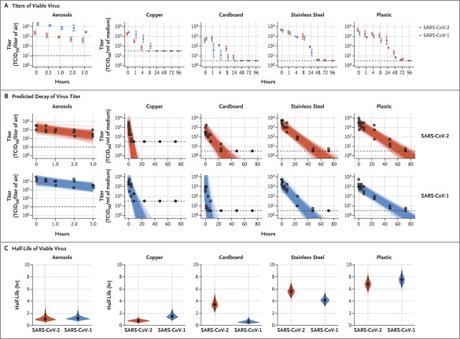
Image description as in van Doremalen et al [2]
As shown in Panel A, the titer of aerosolized viable virus is expressed in 50% tissue-culture infectious dose (TCID 50) per liter of air. Viruses were applied to copper, cardboard, stainless steel, and plastic maintained at 21 to 23°C and 40% relative humidity over 7 days. The titer of viable virus is expressed as TCID 50 per milliliter of collection medium. All samples were quantified by end-point titration on Vero E6 cells. Plots show the means and standard errors (𝙸 bars) across three replicates. As shown in Panel B, regression plots indicate the predicted decay of virus titer over time; the titer is plotted on a logarithmic scale. Points show measured titers and are slightly jittered (i.e., their horizontal positions are modified by a small random amount to reduce overlap) along the time axis to avoid overplotting. Lines are random draws from the joint posterior distribution of the exponential decay rate (negative of the slope) and intercept (initial virus titer) to show the range of possible decay patterns for each experimental condition. There were 150 lines per panel, including 50 lines from each plotted replicate. As shown in Panel C, violin plots indicate posterior distribution for the half-life of viable virus based on the estimated exponential decay rates of the virus titer. The dots indicate the posterior median estimates, and the black lines indicate a 95% credible interval. Experimental conditions are ordered according to the posterior median half-life of SARS-CoV-2. The dashed lines indicate the limit of detection, which was 3.33×10 0.5 TCID 50 per liter of air for aerosols, 10 0.5 TCID 50 per milliliter of medium for plastic, steel, and cardboard, and 10 1.5 TCID 50 per milliliter of medium for copper.
Summary
- The SARS-CoV-2 virus may remain viable on different surfaces for a period of hours to days, although the viral titers may reduce significantly over time, halving in a matter of hours for most surfaces.
- For aerosols
- Significant survival noted till last time point observed (3 hours)
- For plastics
- Viable virus isolated till 72 hours
- Virus titers greatly reduced
- For stainless steel
- Viable virus isolated till 72 hours
- Virus titers greatly reduced
- For copper
- No viable virus isolated beyond 4 hours
- For cardboard
- No viable virus isolated beyond 24 hours
- Modeling exercises also show limited risk of bioaerosols being generated by flushing of toilets. This is significant especially since the virus has been found to be shed in the feces of up to 67% of patients in a case series.
- Although the potential risk of fomite-based transmission remains, US CDC states that this is unlikely to be a major route of transmission.
- If hygiene and surface cleansing with biocidal agents is maintained, risk of transmission may be further reduced. High touch surfaces need special attention.
[1] TCID 50: 50% tissue-culture infectious dose is a method for quantifying viral load. This is the concentration at which 50% of cells in a tissue culture are infected when a test tube or well plate on which the cells have been cultured is inoculated with a diluted solution of the virus. Higher values indicate higher concentration of virus and larger quantum of risk of infectiousness.
References
[2] van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564-1567. doi:10.1056/NEJMc2004973
[3] WHO Coronavirus Disease 2019 (COVID-19) Situation Report 32 (21 February, 2020). Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200221-sitrep-32-covid-19.pdf?sfvrsn=4802d089_2
[4] Li YY, Wang JX, Chen X. Can a toilet promote virus transmission? From a fluid dynamics perspective. Physics of Fluids. 2020 Jun 1;32(6):065107.
[5] Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92(7):833-840. doi:10.1002/jmv.25825
[6] Cai J, Sun W, Huang J, Gamber M, Wu J, He G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg Infect Dis. 2020;26(6):1343-1345. doi:10.3201/eid2606.200412
[7] US CDC: How COVID-19 spreads. Last updated June 16, 2020.
