The Anticoagulant Effect on Active Bleeds
Suppose you have an identified or suspected active bleed. In that case, your doctors need to be aware of the hazard blood thinners pose to your hemosiderin layer. Your body may have taken years to form the coating you have now. Still, if you require an anticoagulant before your bleed is repaired, the consequences could be devastating. Long-term use of a blood thinner is never taken lightly by your medical team. The vast majority of people may only need a short course, but superficial siderosis community members are a special breed. Ordinary is not a descriptive term often used.
Beginning in 2014, when Gary was first diagnosed with superficial siderosis, his neurologist always suspected he had an active bleed. The severity of headaches he was subjected to daily was considered prime evidence. His medical records always contained a warning against any long-term anticoagulant use, even low-dose aspirin. Until an attempt to locate and repair his bleed happened, there was no way to predict the aftereffects of a blood thinner.
One Step Forward Three Steps Back
Even though doctors suspected Gary had an active bleed, chelation kept Gary’s hemosiderin from growing worse. 2014 through 2017, his symptoms were still progressing but at a languid pace. His hearing loss also stayed even for several years. This all changed in 2017 when Gary went in for an ablation procedure.
His heart was beginning to glitch on occasion. A cardiologist referred Gary for a simple procedure to scar a small amount of tissue in the heart and block the abnormal electrical signals, restoring normal rhythm. By now, we know nothing is simple with a superficial siderosis patient. Gary went into a complete heart block on the table, stopping the ablation. An overnight stay turned into a week before he was sent home.
We had been back three days when a feeling of chest congestion left Gary worried pneumonia was developing. A trip to the Emergency Department revealed clots in five lobes of his lung. Multiple pulmonary embolisms found him on a heparin drip and a prescription for an anticoagulant. We voiced our concerns about his active bleed, but a lifetime of blood thinners was needed to keep him from a stroke or even death. A colonoscopy drove the point home when they temporarily suspended his warfarin. He had a DVT before the week was out.
Should We Be Worried?
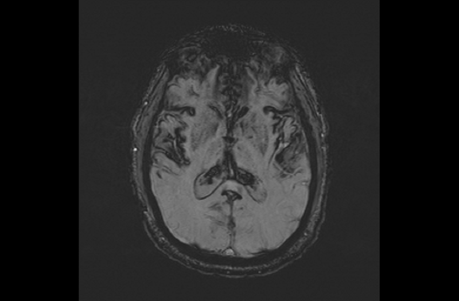
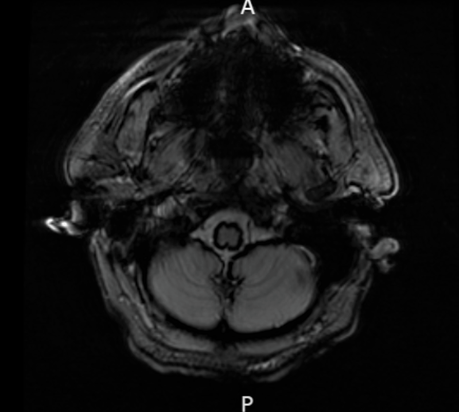
I continued to have serious concerns about the effect a blood thinner was having on the state of Gary’s hemosiderin. A review of his 2018 MRI series was inconclusive due to a higher magnification being used. Visibly, there was a noticeable increase in the area from his earlier scans. Still, until another set could be run, there was no way to be sure. Gary transferred to a new neurologist. I began a serious campaign to have his case reviewed by a new neurosurgery department. The danger seemed too high now that Gary was facing a lifetime of blood thinners.
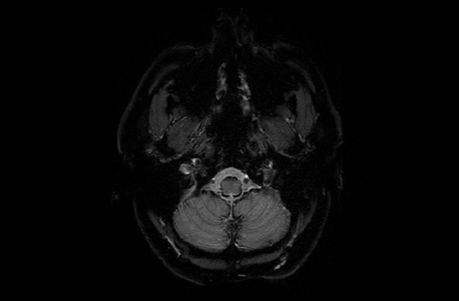
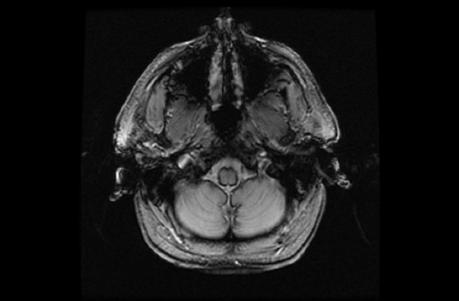
Neurosurgery spent 2019 reviewing his case and getting approval to repair his active bleed. Early in 2020, we were waiting on a date when COVID-19 hit, shutting everything down. You can read more about Gary’s surgery here. His bleed was repaired in March 2021, but his MRI series showed a definite increase in hemosiderin. Areas that had been clear previously are now showing a build-up, with some original areas darker.
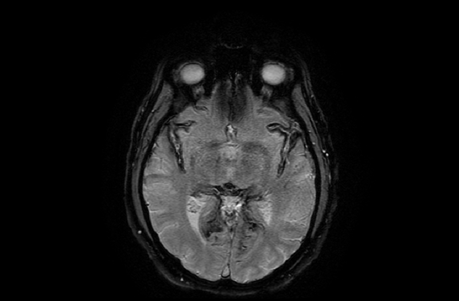
- Dec 2014
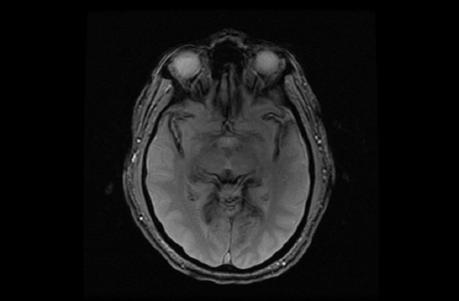
- August 2018
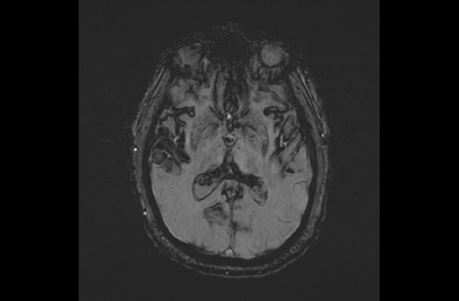
- April 2021
- December 2014
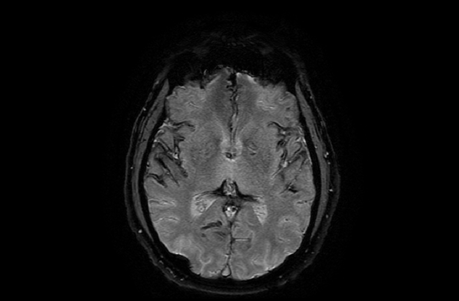
- April 2021
- March 2017
- August 2018
- May 2021
Where To begin
We have decided to take some time to build up the iron levels in his bloodstream before he resumes chelation. While his symptoms have spiraled out of control since 2019, we feel the hemosiderin increase his warfarin use caused has been stopped. The heavier deposits have set him back to ground zero. Hopefully, chelation now has a chance to do more than simply hold the line.

