
What is RBD
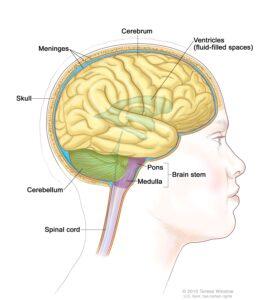
REM Sleep Behavior Disorder (RBD) is a severe secondary condition to neurological disorders in which the pontine areas of the brain controlling REM sleep no longer work correctly. Confirming the disorder requires observing repeated speaking episodes combined with complex movement behaviors during a sleep study. These movement behaviors include hand and arm movement during the REM sleep phase.
Who is Affected
REM Sleep Behavior Disorder affects adults 50+ years and men more than women. While it’s considered an early pre-symptomatic predictor of alpha-synuclein neurodegenerative disorders such as Parkinson’s, Lewy Body dementia, and multiple system atrophy. It has also been diagnosed in non-synuclein neurodegenerative diseases like ALS, Alzheimer’s, spinal cerebellar ataxia type 3, and Huntington’s disease after the patient is symptomatic.
The link between these non-synuclein neurodegenerative conditions is the presence of iron and progressive damage to the brain stem, which interrupts multiple neuronal circuits originating in the pons and ending at spinal cord motor neurons. Chronic anosmia, constipation, and orthostatic hypotension are frequently noted as comorbidities in cases of non-synuclein-related RBD.
There had been, to date, no reports of RBD as secondary to superficial siderosis until now. One identified mid-later stage superficial siderosis patient had received confirmation of the disorder. The Superficial Siderosis Patient Registry will be surveying in 2023 to try and determine if other registry members may be affected.
What Happens?
Typically during REM sleep, the brain sends signals through the neurotransmitter systems across the central, peripheral, and autonomic nervous systems. These signals tell the muscles to relax and enter REM sleep atonia. This pseudo-paralytic state prevents a person from physically acting out dreams. But in people with RBD, these nerve signals don’t work correctly; sleep movement ranges from falling out of bed, and benign hand gestures to violent thrashing, punching and kicking as they act out their dream movements. This can lead to self-injuries, unintentional harm to a sleep partner, or damage to bedroom furniture. The dreams are often highly vivid and may be scary or violent.
Treatment and Saftey Measures
If you or your sleep partner feel like you may be experiencing RBD, you should ask your primary care physician to refer you to a sleep specialist if you are not currently under care. The primary goal is to create a safe space for you and your sleep partner. Extended-release melatonin will often help control movement and is the standard initial treatment.
Safety measures combined with melatonin aren’t enough to prevent injury if your symptoms are severe. In that case, a low-dose prescription benzodiazepine medication may be ordered by your physician.
- Extended-release melatonin one hour before sleep.
- Clear the floor and the area around the bed of any sharp objects.
- Install a bedrail
- Move nearby furniture out of reach (bedside table, lamps, etc.)
- Sleep partners should move to another bed during extreme episodes.

