
Nurse Practitioner (Photo credit: ekea7)
by Amanda Trujillo
If the newer generations of nurses out there are more confused than ever about their roles in healthcare — they should be. I’m one of the newer generations of nurses and I — AM — CONFUSED. Seriously. Think about it. We are taught all of the idyllic, pretty things every good and prudent
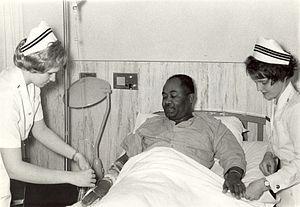
Navy nurses attending to a patient, 1960s. (Photo credit: Wikipedia)
nurse should know and should do whilst caring for patients. The Nurses Code of Ethics is drilled into our heads during nursing school, nursing care plans are celebrated (by our professors of course), and we are championed as the “future” and “promise” of nursing. The beautiful glowing white walls of academia ushers us out of the proverbial nursing nest with a maternal pat on the head, a gentle push, and into the place were supposed to actually do all the stuff were taught and licensed to do, and be who they taught us to be.
You’ve all heard it, I’m sure. “Get out there and make a difference! Change the profession for the next generation! Be the example! Implement policy! Be advocates for your colleagues and your patients!” Ummmm. Yeah. Nurses should act as advocates for not just their patients but for their profession. That being said, let’s take a look at what threatens to unravel the foundational fabric of who we are as nurses and what we do that sets us apart from all other healthcare disciplines.
1. Corporate Nursing. ”We know what nursing is and what nurses do.” However, the moment you walk into the doors of any hospital, the nurse — the persona, and everything else — is redefined according to the wants and expectations and interests of the organization we work for. Nursing, as a discipline, as a science, is redefined. You are who your employer wants and expects you to be. Period. Your own nursing style or “way” of nursing? Leave it at the door, and step into the predefined mold thank you very much. Advanced education? Yeah, that’s great, but you aren’t actually supposed to use it. That MSN is supposed to look good after your name on the plaque that lists all the Masters prepared nurses on the unit you work within. A point of pride that all patients are supposed to gawk at and be impressed by when they walk into the entry way of the nursing unit. I tried using it; I tried to contribute—nope. We just want the letters from you, that’s all.
2. Teeny, tiny amount of autonomy. I mean, come on people. We still have to get orders to ambulate our patients two to three times daily after surgery, to get an incentive spirometer, to initiate pre and post-op teaching, and even to monitor ins and outs every four hours. Every state has a different nurse practice act, and there is no set regulation as to what nurses can and cannot do across the United States. Every state defines Nurses and their practice and what they can do differently. Take a group of 5 doctors—and chances are each one of them don’t even have a good understanding of what nurses are and what they do and their role. Interdisciplinary Models of Care are not the standard yet, so this inhibits a productive and working knowledge of what each provider does.
3. Disregard for Care Plans. This is a big one for me. I recently read a couple of articles that, for the most part, said care plans should just die and go by the wayside because they are useless.
4. A fractured profession. We have so many specialties that we still have failed to come together in a unified manner to advocate together for our profession and for the vital role we play in the lives of our patients, evidence based practice, theory development and application, and policy making. The result? Thousands of different visions from thousands of different nurses about what our profession “should be” and “should do.”
5. Silencing of our voices. We now have to choose between our own career survival, or own livelihoods, professional reputations, and paychecks—and speaking up in the best interests of our patients. Many a nurse has experienced this tragic conundrum, and the consequences are well documented if you log into your university libraries and do a good literature review on the topic. So, which will it be? Your pay check or your patient’s life? Well, now, that depends—can you like yourself when you go to sleep at night or when you wake up the next morning. The choice will be different for all of us.
6. Too many initiatives!!!! There are so many initiatives out there that it truly is like ‘herding cats’ to get everyone on the same page about what needs to bedone to improve, advance, and grow our profession.

The American student nurse Miss Lydia Monroe of Ringold, Louisiana, in 1942. (Photo credit: Wikipedia)
What I feel needs to be done is simply this: get back to basics. All the initiatives are great. The pretty, flowery, shiny, idealistic profession they propose is in theory—just that. It seems like every time we turn around there is another nursing initiative being introduced. In fact, there are so many, we all seem to have thrown up our stethoscopes in exasperation while uttering “Whatever.” The RWJF, the NIH, AACN, the National League for Nursing, Johnson and Johnson, the Institute of Medicine and all the other organizations that produce the massive documents proposing their positions on where nursing should be by the year “such and such” need to set aside “Candyland” and get back to the drawing board.
How? Perform a learning assessment and care plan on the profession. TALK TO THE NURSES AT THE BEDSIDE—these are the stakeholders that have to carry out all the grandiose changes. ASK nurses what would motivate them to carry out change and what they need or want to learn to carry out the change. Perform a force field analysis to illustrate whether there is a greater push for or against change and where a balance can be achieved to promote success. What do nurses consider an incentive to participate in the change process? What is their currency?
Here is a good example of what happens when big organizations try to make even bigger changes sans discussion with their staff members, which is to say, their stakeholders. At one hospital I worked at the Transforming Care At The Bedside Initiative was being “enforced” as a means to improve patient satisfaction scores. I say the word “enforced” because we nurses weren’t asked about how we felt about it, we weren’t “completely” educated about what TCAB was, why we should be interested in it, or why we should participate in it. participation was an expectation and people were “assigned” to do parts of the initiative. No communication took place between management and staff about how they felt about the change process or the new “tests of change” they were being expected to participate in. So, it was not a big surprise to see my coworkers increasingly annoyed when they were being presented with “more steps” in their workday, or “more papers” to fill out or “scripts” taped to their computer monitors directing what they were to say to their patients. It was also not surprising to see that few or no staff members were attending the TCAB meetings to provide input and feedback.
Having gotten my Masters Degree I quickly realized what was missing was a well-planned approach to the change process. A crucial step within the change process is involving every person that could possibly be involved in that change: polling people, studying your stakeholders and what their motivations are, illustrating what is ‘in it for them’ should they take part. Failing to study all of your stakeholders and ask for feedback prior to initiating change is simply wasting a lot of time and yelling through a megaphone at an empty nursing station. I did some further research into the TCAB Initiative by immersing myself in the RWJF website for a couple of weeks.
After doing so, I discovered that our organization was not implementing TCAB as it was meant to be implemented. The organization was taking bits and pieces of the initiative and implementing them. The focus of the initiative — promoting happy nurses to promote happy satisfied patients — was not the managerial focus, as it should have been. It was strictly designed for patients, completely overstepping the spirit of the TCAB initiative as it was meant to be implemented. Lastly, the TCAB initiative was designed to be an interdisciplinary effort. The way it was being pushed at the organization I was at, the focus was just on nurses. I put together a white paper and power point and submitted them to my manager hoping it would help to get the project on track. I was promptly shut down with an annoyed response that my work looked plagiarized. (This is what an MSN on a nursing floor gets you)
So, managers, here are some lessons learned. If you want to make change on a large scale you must invest the time, no matter how long or how involved the effort, to study the people who have to carry out the work. Find out their goals, wishes, motivations, concerns, what makes them happy, angry, and frustrated. Find out what their knowledge base is and what must be learned to carry out the major initiative. Ask for their input. Discover who your “downers” are, why they are resistant to change, and how can you get them on board. It’s called “buy in.”
Lastly, harvest your talent. Take a fresh look at who your voices and cheerleaders are on the unit and give them “room to bloom where they are planted.” This is how and where you become a transformational leader instead of a leader who suppresses the creativity and potential of your nursing staff. One note: if you are going to implement something huge like the RWJF TCAB Initiative, don’t just take pieces of it and throw together your own version and expect it to work.

(Photo credit: Wikipedia)
This, in my opinion, is what all of the large nursing organizations who want to transform healthcare need to do. Round everybody up for a week-long conference, every stakeholder — not just administration and management figures or politicians either. The real people: the bedside nurses, pharmacists, lab workers, patients, doctors, PA’s, housekeepers and so on. Paint the closest picture you can get to a collective vision everyone seems to share. Then, figure out how to get there, one step at a time.
All the big goals are great.I love the visions of where the RWJF and the IOM and the AACN see our profession, healthcare, and nursing education headed. But the visions are a problem too. There are too many ideas, initiatives, and too many people “other than bedside nurses” generating them. Our profession is fractured enough. It is not feasible, nor is it realistic, to expect every wonderful idea and vision to be carried to fruition when there is currently a longstanding lack of unity and disarray within nursing.
So, for the time being, let’s set aside the huge mountain of ideas and initiatives and take a deep breath. Now, start over with the A-B-C’s: Airway, Breathing, Circulation. Set the sights on resuscitating the profession of nursing first, before we attempt to heal the ailing healthcare system and the world. Take it back to the old school, and do the assessment first. Then, make a plan: implement it, evaluate it, and do it all over again until we get nursing back on track with a unified focus. Only THEN can we climb the mountains set in front of us by the RWJF or the IOM or the NIH. We cannot build castles without a strong foundation of earth below it.
By the way . . . Did anyone notice how often I used the word “initiative?”
__________
Amanda blogs at NurseInterupted. This is a slightly modified version of a post which originally appeared on her blog.
