Health benefits of moderate drinking come under fire.
One of those things that “everybody knows” about alcohol is that a drink or two per day is good for your heart. But maybe not as good for your heart as no drinks at all.
Joint first authors Michael V. Holmes of the Department of Epidemiology and Public Health at University College in London, and Caroline E. Dale at the London School of Hygiene & Tropical Medicine in London, recently published a multi-site meta-analysis of epidemiological studies centering on a common gene for alcohol metabolization. The report, published in the UK journal BMJ, brings “the hypothesized cardioprotective effect of alcohol into question,” according to the authors.
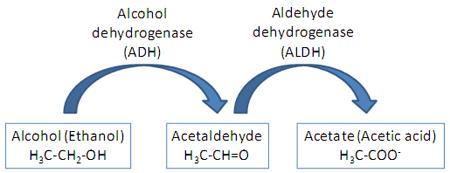
People who are born with a particular variant in the gene controlling for the expression of alcohol dehydrogenase, the major enzyme involved in converting alcohol into waste products, will show the familiar flush reaction when they drink. Alcohol, literally, can make many of them sick. This genetic variant, in combination with other enzymes, can be strongly protective against alcohol, and is much more commonly found among Asian populations. Roughly 40% of Japanese, Korean, and Northeastern Chinese populations show the characteristic “Asian glow” to one degree or another if they choose to drink. (One reason why this effect isn't better known is that the condition is close to nonexistent in Westerners).
People with this alcohol dehydrogenase deficiency, the researchers found, not only consume less alcohol, for obvious reasons, but “had lower, not higher, odds of developing coronary heart disease regardless of whether they were light, moderate, or heavy drinkers.” Here are the conclusions in detail: “Carriers of the rs1229984 A-allele had lower levels of alcohol consumption and exhibited lower levels of blood pressure, inflammatory biomarkers, adiposity measures, and non-HDL cholesterol, and reduced odds of developing coronary heart disease, compared with non-carriers of this allele.”
The authors conclude that "reduction of alcohol consumption, even for light to moderate drinkers, is beneficial for cardiovascular health.”
How does this work? The researchers aren’t completely sure, but note that the “most widely proposed mechanism” is an increase in high-density lipoprotein (HDL) cholesterol. “Although an HDL cholesterol raising effect of alcohol has been reported in experimental studies, the small sample size and short follow-up means existing studies may be prone to bias,” thereby limiting their usefulness. Moreover, the BMJ study itself found “no overall difference between allele carriers and non-carriers in HDL concentration.”
Like most meta-studies, this one has its strengths and weaknesses. The study used a large sample size, used detailed alcohol phenotypic data, and didn't have to deal with the inherent biases of observational-type studies. On the minus side, the lack of a connection between the allele in question and HDL levels is troubling, and stroke data was lacking.
But overall, the authors believe that "social pressure in heavier drinking cultures is unlikely to override the effect of the genetic variant on alcohol consumption."
In retrospect, there have been some trouble spots along the way: A 2008 study in Current Atherosclerosis Reports concluded:
In the absence of large randomized trials of moderate alcohol consumption and heart failure, we cannot exclude residual confounding or unmeasured confounding as possible explanations for the observed relationships. Thus, for patients who do not consume any alcohol, it would be premature to recommend light-to-moderate drinking as a means to lower the risk of heart failure, given the possible risk of abuse and resulting consequences.
At present, the American Heart Association does not recommend drinking any amount of wine or other alcoholic beverages in order to gain potential health benefits.
Holmes M.V., L. Zuccolo, R. J. Silverwood, Y. Guo, Z. Ye, D. Prieto-Merino, A. Dehghan, S. Trompet, A. Wong & A. Cavadino & (2014). Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data, BMJ, 349 (jul10 6) g4164-g4164. DOI: http://dx.doi.org/10.1136/bmj.g4164
Photo credit: http://qsystem.gblifesciences.com/

