Are you looking for fast and effective ways to lose weight or treat type 2 diabetes? You may have heard of weight loss surgery, also called bariatric surgery - which is proven to be effective for weight loss and metabolic improvements. But is it right for you?
In this guide, we'll teach you about the potential benefits and drawbacks of weight loss surgery - as well as the therapeutic role of nutrition.
We incorporate the latest evidence and draw on the clinical experience and practical advice of two experienced weight loss surgeons, Dr. Ariel Ortiz and Dr. Meredith Sweeney.
After reading this guide, you'll have a better understanding of the pros, cons, and potential alternatives to weight loss surgery.
Start your FREE 30-day trial!
Get instant access to healthy low-carb and keto meal plans, fast and easy recipes, weight loss advice from medical experts, and so much more. A healthier life starts now with your free trial!
Start FREE trial!
1. What is weight loss surgery?
Weight loss surgery, also known as bariatric surgery, is a major operation that changes the anatomy of the stomach and intestines. It makes it harder to eat and digest large quantities of food.
Surgeons perform bariatric surgery laparoscopically, making multiple small incisions through which they insert a camera and all the tools to operate.
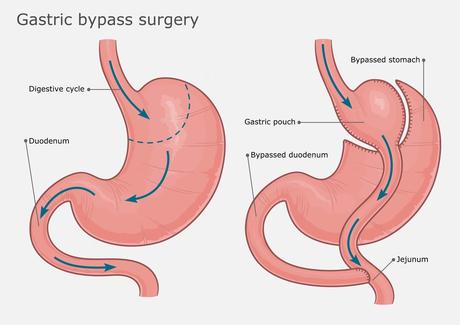
The two most common surgeries are the gastric bypass and the gastric sleeve. The gastric bypass, as the name suggests, "bypasses" the stomach and upper small intestine. The surgeon creates a new, smaller stomach during this procedure.
For the gastric sleeve operation, doctors reduce the size and structure of the stomach to be similar to the esophagus, without needing to create a new stomach or bypass part of the intestines.
The gastric bypass is a longer, more complex operation compared to a gastric sleeve. Although gastric bypass may produce more significant weight loss, findings are inconsistent. Dr. Ortiz feels any difference is likely negligible since the gastric sleeve is a much simpler and shorter operation that still results in dramatic weight loss.
Newer, less invasive options include inflatable balloons, funnels or stents placed in the stomach. These procedures are designed to decrease the size or function of the stomach. Since these techniques are new, data on their long-term success is limited.
Summary
Weight loss surgery, also known as bariatric surgery, limits the size of the stomach (both sleeve and bypass operation) and the ability to absorb nutrients (bypass surgery). Some techniques also involve bypassing the upper part of the small intestines. Gastric bypass and gastric sleeve operations are the most commonly performed procedures.
2. Weight loss success with surgery

Both gastric bypass and the gastric sleeve are effective for weight loss. A randomized trial found that gastric bypass patients maintained 24% weight loss three years after surgery, with gastric sleeve patients maintaining 21% weight loss.
Another study of 417 patients undergoing gastric bypass reported 35% weight loss from their baseline at two years and patients gained back some weight but maintained 27% weight loss at 12 years.
Most of the evidence agrees with these studies and shows significant weight loss with bariatric surgery.
However, not every patient sees success. One review paper estimates the failure rate of gastric bypass as 20-35%. Failure was defined as achieving less than 50% excess weight loss or having a BMI greater than 35.
In addition, weight gain is common 18 months after surgery, with approximately 50% of patients regaining some weight.
Summary
Weight loss surgery is an effective way to lose 25 to 30% of baseline weight and keep it off for 12 years. Most patients see long-term success, but roughly 26% remain obese even after surgery. Regaining some weight is common after 18 months.
3. Metabolic benefits of weight loss surgery

In addition to weight loss, bariatric surgery delivers profound benefits for metabolic health, so much so that many physicians now refer to it as "metabolic surgery."
An influential study looking at the effects of bariatric surgery on type 2 diabetes randomized 150 patients with this condition and an average hemoglobin A1c (HbA1c) - a measure of average blood sugar - of 9.3% into three groups: diabetes medications alone, gastric bypass surgery, or a gastric sleeve procedure.
After three years, researchers found an HbA1c of less than 6.0 in just 5% of medical therapy patients, as opposed to 38% in gastric bypass patients and 24% in gastric sleeve patients. The surgery patients also achieved much greater weight loss, at 24% of body weight compared to just 4% for the medical therapy group.
Other studies confirmed these findings with similar results.
As Dr. Ortiz notes, most patients experience rapid improvement in blood sugar control and can stop their diabetes medications well before any significant weight loss occurs. This raises a question: If weight loss alone is what causes improved blood sugar control, how do we explain it occurring so quickly, before meaningful weight loss?
Nevertheless, some studies suggest that metabolic benefits of bariatric surgery track well with weight lost over the long term.
One small study matched patients with 18% weight loss from lifestyle intervention with similar patients who had weight loss surgery. The results suggest that for improvement in HbA1c and insulin sensitivity, there was no significant difference between the two groups.
But not all surgeries are the same. For instance, one study reported those undergoing gastric bypass had greater diabetes remission after seven years compared to those undergoing gastric banding.
What about longevity?
With improved weight loss and diabetes remission, can weight loss surgery help patients live longer? The current body of evidence suggests that it can.
A Swedish study reported a 24% relative reduction in death at 10 years in those who had surgery compared to a control group.
And a 2020 meta-analysis suggests a 38% reduction in death rate for those who had surgery.
However, there was a drastic difference in weight loss between the surgical group and the control group in these analyses.
For example, in the Swedish study, the surgery group lost an average of 24% of their body weight, but the control group experienced a small weight gain. It is unknown if there would have been any longevity benefit for patients undergoing weight loss surgery compared to a group that achieved similar weight loss through diet and lifestyle.
We can conclude that weight loss surgery can improve mortality and improve weight loss and metabolic health. But we can't say if surgery has additional benefits compared to similar metabolic and weight improvements achieved by other means.
Summary
Weight loss surgery is effective at improving blood sugar control and even at reversing type 2 diabetes. Experts have different opinions about whether the benefits result from weight loss alone or are due to something unique about the surgery itself.
Studies suggest improved longevity after bariatric surgery, but it is unknown whether people who achieved similar and lasting weight loss by other means would have similar improvements in longevity.
4. Role of nutrition

Nutrition, by itself - especially low-carb nutrition - can be an effective way to achieve significant weight loss. For those who undergo weight loss surgery, nutrition plays an integral role in both preparing for surgery and improving long-lasting success after surgery.
It's no secret that some people regain a significant amount of weight after weight loss surgery. As Dr. Sweeney states, surgical issues are rarely to blame for weight regain. Instead, the most common cause is a return to old eating habits.
As a rule, it helps to approach weight loss surgery as a kick start to a new lifestyle. The surgery helps with rapid weight loss, but patients keep the weight off through smart lifestyle choices.
Drs. Ortiz and Sweeney both promote very low-carb diets for their surgical patients. They believe low-carb diets offer sustainable weight loss while providing enough protein and micronutrients.
Dr. Sweeney feels the importance of nutrition becomes more of a priority about two years after surgery. "I like to tell my patients they have two years to figure their diet out because that is when people start to see regain without significant lifestyle improvements."
Additionally, Dr. Sweeney recommends intermittent fasting, but only after the patient has completely healed from the surgery and consistently following a low-carb diet. She believes short-term fasting and time-restricted eating can play an important role in long-term weight maintenance, but starting too early is problematic for many patients.
Nutritional support isn't only needed after the surgery. Dr. Ortiz emphasizes how well pre-operative intermittent fasting and low-carb nutrition work for preparing his patients for surgery.
Most of Dr. Ortiz's patients have fatty liver disease. This makes it more challenging to perform the operation since an enlarged liver "gets in the way" during surgery.
Dr. Sweeney agrees, saying that it is much easier to perform the surgery when the liver is not enlarged. That's why she puts all her patients on a "liver-shrinking diet," featuring time-restricted eating and low-carb nutrition.
Fortunately, patients can improve fatty liver with only a few days to a few weeks of dietary changes. Studies of very low-calorie diets confirm those findings, although studies of low-carb diets as a pre-surgery intervention have not been done.
Long-term nutrition therapy
Long-term micronutrient or even protein deficiencies may be a concern with weight loss surgery.
Official guidelines for clinicians recommend all patients undergo nutritional screening before and after surgery and that clinicians prescribe supplements based on the type of surgery performed.
For instance, iron and vitamin B12 deficiencies occur in up to 50% of patients who have gastric bypass surgery, but these are much less common with other surgical techniques.
Vitamin D, calcium, and protein deficiencies can occur with any weight loss surgery, although they are less common than iron and vitamin B12 deficiencies.
For long-term health, many experts recommend ensuring patients eat enough protein. At Diet Doctor, we define moderate protein intake as 1.2 to 1.7 grams per kilo of reference body weight per day. You can read more about our protein recommendations in our evidence-based guide.
Clinical guidelines also suggest life-long supplements after bariatric surgery.
Summary
Nutrition plays a vital role before and after surgery. Although there are no trials comparing low-carb diets to other diets after weight loss surgery, bariatric surgeons' clinical experience suggests low carb is an effective and sustainable diet.
Any nutrition plan should aim to prevent protein, vitamin, and mineral deficiencies.

