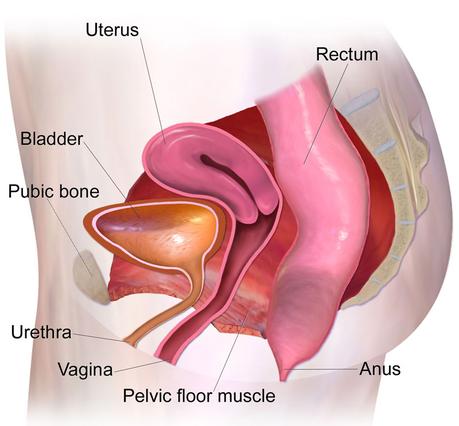
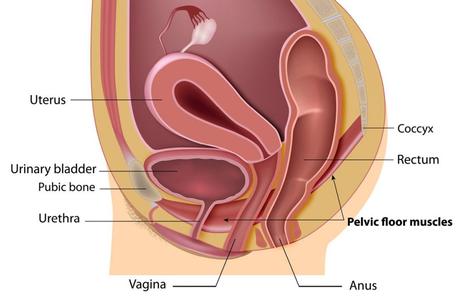
The pelvic floor is a collection of muscles and ligaments in the pelvic region that act as a chain to protect the pelvic organs, including the bladder, rectum, uterus, or prostate. The contraction and relaxation of these muscles allow the control of bowel movements, urination, and especially for women to have sex. Inability to control the pelvic floor muscles is called pelvic floor dysfunction. Impaired pelvic floor function forces the patient to contract muscles. As a result, they may have trouble defecating. Pelvic floor dysfunction, if left untreated, can lead to discomfort, long-term colon damage, or infection.
What Are the Symptoms of Pelvic Floor Dysfunction?
Symptoms associated with pelvic floor dysfunction include:
- Urine issues, such as inability to control or painful urination
- Constipation
- Low back pain
- Pain in the pelvis, genitals, or rectum
- Discomfort during sex for women
- Pressure in the pelvis or rectum
- Muscle spasm in the pelvis
What Causes Pelvic Floor Dysfunction?
While the exact cause of pelvic floor muscle dysfunction is unknown, doctors have found a link between the disease and conditions or events that weaken the pelvic floor muscles or rupture connective tissue. The following are some of the factors that can impair the function of the pelvic floor muscles:
- Giving birth
- Traumatic injury in the pelvic area
- Obesity
- Pelvic surgery
- Nerve damage

Diagnosis of Pelvic Floor Muscle Dysfunction
A person needs to be able to recognize the symptoms of the disease. Sometimes, some symptoms indicate more serious problems. To diagnose, the doctor first examines the patient’s medical history and examines the symptoms. After the initial consultation, a physical examination is needed to look for muscle or nodal spasms. This examination also examines muscle weakness. To monitor how the pelvic floor muscles and pelvic muscle contractions are monitored, your doctor inserts a perineometer into the patient’s rectum or vagina. The perineometer is a small device and sensor that can be used to perform internal examination.
A less invasive procedure is to place electrodes on the perineum, the area between the scrotum and the anus, or the vagina and anus to determine if the patient can contract or relax their pelvic floor muscles.
Types of Pelvic Floor Disorders
Obstructed defecation: Obstruction is difficulty moving the bowel and passing stool. Obstruction of the bowel may be caused by sagging pelvic floor organs (intestine, uterus, and bladder) or abnormal function (spasm) of the pelvic floor muscles. In this disease, the stool reaches the end of the intestine, but the patient has difficulty passing stool. If you have this problem, you will feel incomplete defecation, as if feces remained in the rectum.
Rectocele (prolapse of the large intestine): The rectocele is a protrusion in the anterior wall of the end of the large intestine (rectum) toward the vagina. Normally, the rectum attaches directly to the anus. When a patient with a rectocele strains to defecate, the stool may become trapped in an abnormal protrusion of the rectum that protrudes toward the vagina. This problem prevents complete defecation. Rectocele usually does not cause symptoms in the early stages. As the bulge grows and the disease progresses, defecation becomes difficult for the patient, and there may be some stool leakage (stool incontinence) with bowel movements. Rectocele is more common in women who have given birth than men. The cause of the rectocele is usually due to the weakness of the pelvic floor muscles and the thinning of the tissue between the rectum and the vagina. Early and undeveloped stages of rectocele can be treated with pelvic floor physiotherapy and biofeedback.
Pelvic floor prolapse: As mentioned earlier, the pelvic floor consists of muscles, ligaments, and organs such as the rectum, vagina, and bladder. Stretching and pressure on the pelvic floor elements may occur with age or after childbirth. Symptoms of the disease usually include difficulty urinating completely or difficulty passing stools, incontinence, or a feeling of pressure in the pelvic area. Depending on the degree of descent of the organ, the falls are divided into several degrees. Mild prolapse in which an organ (uterus, bladder, or end of the large intestine) has not protruded from the vagina or anus is treated with pelvic floor physiotherapy and biofeedback.
Functional constipation Dyssynergic defecation: or paradoxical puborectalis muscle contraction: The prevalence of constipation in the community is about 11%, of which more than 50% have dysinergic excretion. The puborectalis muscle is part of the muscular control of defecation. This muscle is wrapped around the end of the rectum like a hook. The puborectalis muscle should relax during bowel movements to allow bowel movements with bowel movements. If this muscle does not relax or tighten due to inconsistent contraction, you feel like pushing a closed door when you push for defecation. A proven and permanent treatment for this type of constipation is pelvic floor physiotherapy and biofeedback.
Coccyalgia: The coccyx is the small bone at the end of the spine. Coccygeal pain is the pain of this bone. The pain usually gets worse with prolonged movement and sitting, and in some cases, there is pain when the patient defecates.
Pelvic floor muscle spasm syndrome: This syndrome is pelvic floor muscle spasm. Spasms may occur after bowel movements or for no apparent reason. Patients often have long periods of high and ambiguous pressure in the distal region of the large intestine. These symptoms may get worse when sitting or lying down. Pelvic floor spasms are more common in women than men.
Treatment of Pelvic Floor Dysfunction
The goal of treatment for pelvic floor dysfunction is to relax the pelvic floor muscles to facilitate bowel movements and greater control. In addition to surgery, there are less invasive methods for treating this disorder. Kegel exercises or similar methods requiring a person to contract muscles are ineffective for this disease.
Treatment depends on the cause of the disorder and the severity of your symptoms. In most cases, non-invasive treatments such as pelvic floor physiotherapy solve the patient’s problem. Fortunately, surgical treatment is necessary only in rare pelvic floor disorders such as severe prolapse (protrusion of the uterus or bladder out of the vagina).
A common treatment for this disease is biofeedback. In this method, the therapist can control the relaxation or contraction of the pelvic muscles through special sensors. After observing muscle activity, the therapist tells the patient how to improve their coordination. Other treatment options include:
Medicine:
Your doctor may prescribe a muscle relaxant to help relieve the symptoms of pelvic floor dysfunction. Relaxers prevent muscle contraction.
Self-care:
To reduce the pressure on the pelvic floor muscles, you should avoid pushing or forcing in the bathroom. Relaxation techniques such as yoga and stretching exercises help relax the pelvic floor muscles. Using a hot bath is another useful method. Hot water improves blood circulation and relaxes muscles.
Surgery:
If the pelvic floor dysfunction is due to a sagging rectum, surgery can loosen the damaged pelvic organs. Rectal prolapse is a condition that causes anal tissue to fall into the anus.
Pelvic floor physiotherapy and use of biofeedback:
This treatment, performed by a specialized and trained pelvic floor physiotherapist, aims to improve the sensation of the rectal area and strengthen and/or relax the pelvic floor muscles. This method uses electrical stimulation, biofeedback, shockwave, training, special exercises, laser therapy, and specialized manual therapies. According to research, biofeedback has been effective in more than 70% of patients with constipation and pelvic pain, and its therapeutic results remain stable for up to 2 years after recovery. For more information, you can read the article Pelvic floor physiotherapy on this site.
Conclusion:
Pelvic floor dysfunction can be treated, although it is uncomfortable or sometimes painful. Try several home remedies before resorting to medication or surgery for treatment. Talk to your doctor about your symptoms so that the problem can be diagnosed correctly.

