How Is Sleeve Gastrectomy Performed?
The laparoscopic sleeve gastrectomy is a surgical weight loss procedure performed to reduce the stomach size by about 25% of its original size. This procedure will reduce the stomach size permanently and this an irreversible procedure.
During this procedure, your surgeon will make a longitudinal resection of the stomach beginning from the antrum at the point 5 to 6 cm from the pylorus and ending at the fundus closer to the cardia. This results in a tube or sleeve like structure which is calibrated with a bougie. Often the surgeons prefer using a bougie of 36-40 Fr with this procedure. The ideal remaining size of the stomach post sleeve gastrectomy is nearly 150mL.
In this procedure, the doctor will make five or six small incisions in the abdomen and then insert a video camera called laparoscope through these incisions. LSG (Laparoscopic Sleeve Gastrectomy) takes nearly one to two hours to complete.
How Does Sleeve Gastrectomy Cause Weight Loss?
This is a restrictive procedure which greatly reduces the size of your stomach such that it limit the amount of food to be eaten at a time. This procedure does not reduce the absorption of the nutrients instead you’ll feel full very quickly after eating a small amount of food.
Patients who undergo this procedure will have decreased appetite. Sleeve gastrectomy will reduce the size of the stomach as well as decrease the production of “hunger hormones” by the stomach. Thus, the laparoscopic sleeve gastrectomy will contribute to weight loss.
How Much Weight-loss Occurs after LSG?
The amount of weight loss in the region is about 70% of excess weight. Often this weight loss occurs over the period of the first 9 to 12 months post LSG. Patients who had undergone this procedure should adopt healthy eating habits and should follow physical activity to achieve excess weight loss.
Who Need to Undergo Laparoscopic Sleeve Gastrectomy?
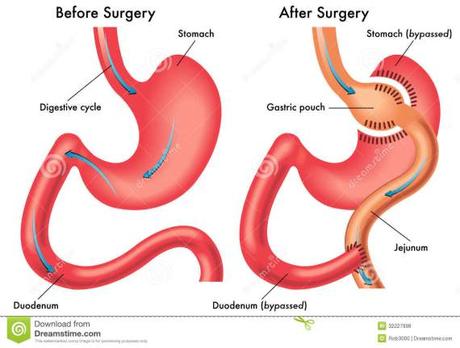
Usually, sleeve gastrectomy is performed as a part of a two staged approach for a surgical weight loss. Later this procedure was performed as first part of the two stage bypass operation on extremely obese patients for whom the risk of performing the gastric bypass surgery was higher.
Patients having higher body mass index (BMI) or who are at higher risk for longer procedure due to lung or heart problems or who are at risk to undergo anesthesia will benefit from LSG.
Risk Factors of Laparoscopic Sleeve Gastrectomy:
The risks of LSG are rare and major complications are reported less than one percent. Some of the common risks of Laparoscopic sleeve gastrectomy include infection and bleeding. The operative risks for LSG is lower than the risks related to gastric bypass.
Benefits of Laparoscopic Sleeve Gastrectomy:
- In this procedure, the function of the stomach is preserved because the nerves of the stomach and the outlet valve are not altered.
- It significantly decreases the hunger by removing the part of the stomach which produces the hunger stimulating hormones.
- It allows the normal food ingestion which results in reduced risk for developing lack of minerals and vitamins as well as eliminates the dumping syndrome.
- Reduce the risk for developing ulcers.
- More than 75% of patients undergoing LSG have reported improvement in hypertension, abnormal cholesterol levels, diabetes and obstructive sleep apnea.
Is Laparoscopic Sleeve Gastrectomy A Good Choice For Me?
Today, the laparoscopic sleeve gastrectomy is the fastest growing and effective weight loss surgery. This surgery is more effective as compared to the gastric bypass surgery for weight loss. It is advised to talk with your doctor to understand about this procedure.
References:
- Paluszkiewicz R, Kalinowski P, Wróblewski T et al. (December 2012). “Prospective randomized clinical trial of laparoscopic sleeve gastrectomy versus open Roux-en-Y gastric bypass for the management of patients with morbid obesity”. Wideochirurgia I Inne Techniki Mało Inwazyjne 7 (4): 225–32
- Karmali S, Schauer P, Birch D, Sharma AM, Sherman V (April 2010). “Laparoscopic sleeve gastrectomy: an innovative new tool in the battle against the obesity epidemic in Canada”. Canadian Journal of Surgery 53 (2): 126–32.

