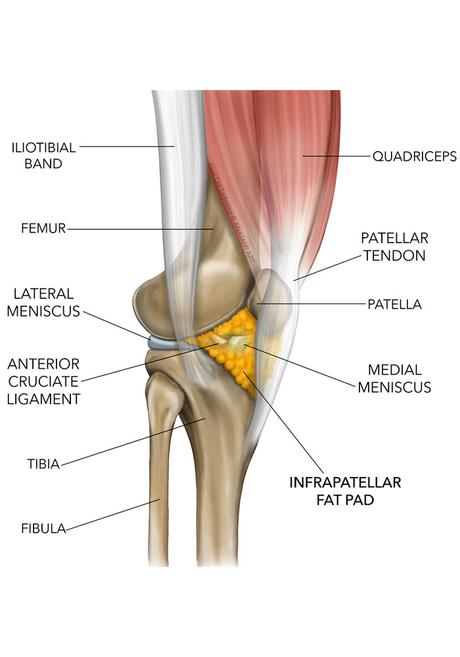
Infrapatellar fat pad syndrome; Infrapatellar Fat Pad or Hoffa Pad is a soft tissue located under the patella and behind the patellar tendon. The infrapatellar fat pad is a shock absorber and protects the femoral condyle (or end of the femur) in the event of a direct blow to the front of the knee. It also reduces the friction between the patella, the saphenous nerve, and the bony structure of the knee.
The fat pad of the knee has many nerve cells, so any damage to it is very painful. Acute or chronic inflammation of the infrapatellar fat pad is called fat pad syndrome or Hoffa syndrome, which is a common cause of front knee pain.
The rate of prevalence of this disease in women is up to 3 times that of men and the highest prevalence of the disease is between the ages of 40 and 60 years. Jumping sports and ligamentous laxity are risk factors.
Causes of Infrapatellar Fat Pad Syndrome
The irritation and inflammation of the fat pad in the knee may be acute or chronic and can be caused by the following reasons:
- Impact on the front of the knee due to trauma or falling
- Excessive sports activity
- Anterior cruciate ligament (ACL) injury reduces knee stability and makes the infrapatellar fat pad more susceptible to injury.
- People with a history of knee hyperextension or genu recurvatum
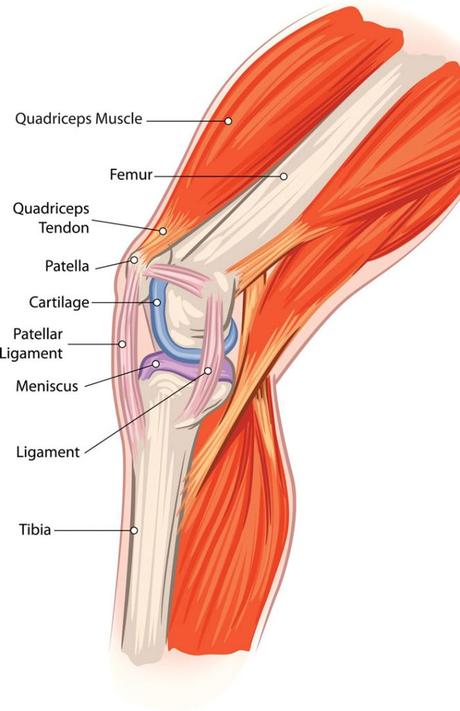
- Quadriceps stiffness
Symptoms of Infrapatellar Fat Pad Syndrome
Symptoms of an Infrapatellar Fat Pad injury include:
- Pain, inflammation, and swelling in the front of the kneecap and on both sides of the patellar tendon.
- Sensitivity to touch at the bottom and below the kneecap
- Increased pain in knee extension (straightening).
- Increased pain when standing for a long time
- Increased pain when squatting or going downstairs
How Long Does Fat Pad Syndrome Take to Heal?
Most people will recover in 8 to 12 weeks, but in some cases, it can take up to 6 months to fully recover. Repeated fat pad impingement, personal biomechanics, and the individual’s conditioning will affect recovery time.
Diagnosis of Infrapatellar Fat Pad Syndrome
Physical examination
Physical examination and careful examination of the knee by an orthopedic specialist
Hoffa test
It is an evaluation method that includes the movement of the kneecap during the contraction of the quadriceps muscle. In this test, the doctor asks the patient to lie with the knee bent (30 degrees), then slowly straighten his leg while the doctor presses his fingers under the patella and on the lateral border of the patellar tendon on both sides. Any pain or tenderness when straightening the leg is a positive test for Hoffa syndrome.
MRI
Used to evaluate the pathology of infrapatellar fat pad syndrome including fibrosis, inflammation, and edema.
What Causes A Migraine Tennis elbowWhat Tests Confirm Hoffa Syndrome?
If you are concerned that you may have Hoffa syndrome, it is best to see a physical therapist or sports medicine doctor so that they can perform a thorough examination of the knee and associated movement patterns.
Doctors perform the Hoffa test, which is an assessment method that involves the movement of the kneecap while contracting the quadriceps muscle. Although MRI can be used to diagnose inflammation, MRI cannot show the root of the problem. Only an experienced doctor can assess the root of the problem and provide a treatment method.
Treatment Methods of Infrapatellar Fat Pad Syndrome
The goal of treatment is to reduce pain, improve knee strength, and prevent further injuries.
The doctor offers a specific treatment plan based on the injury mechanism. Since this complication is considered an inflammatory disease, non-surgical treatment methods are usually used to reduce inflammation, which includes the following:
- Using a cold compress is very useful for relieving acute symptoms and reducing inflammation (ice can be used for 10 minutes every hour)
- Avoiding activities that cause pain and excessive pressure on the knee
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain, inflammation, and swelling
- Physiotherapy and quadriceps strengthening exercises and quadriceps and hip extensor stretching exercises
- Ultrasound, and local laser therapy to increase blood supply and strengthen tissue
- In some cases, corticosteroid injections may be given around the knee to provide temporary pain relief
- Taping: with tape to close the upper surface of the patella to provide more space for the structures below the lower surfaces, i.e. the fat pad, and be under less pressure.
- If conservative treatments do not work, the fat pad may be partially removed with arthroscopic surgery.

Prevent Fat Pad Syndrome
The best way to prevent the occurrence or recurrence of fat layer syndrome is to increase the strength and flexibility of the muscles around the knee, hip joint, and ankle.
A corrective movement specialist is a person who guides the person toward the best exercises to correct the defects in these areas.
If you’ve already struggled with anti-fatigue, it’s best to avoid activities that aggravate the injury, such as squatting, squatting, and kicking for long periods. For women, it is better to limit walking with high heels.
Physiotherapy for Hoffa’s Fat Pad Impingement
Activity modification is the most effective way to help settle the irritation and pain of a fat pad impingement by avoiding hyperextension and reducing activities that aggravate your pain. Targeted stretches and massage to the muscles around the knee, such as the quadriceps, hamstring, and calf, can be helpful, and over-the-counter anti-inflammatories can also help.
From your assessment, your physical therapist should understand what has caused you to develop an inflamed fat pad. They should also understand what factors might be continuing to irritate them that are specific to you and therefore what modifications you need to make.
For long-term resolution, it is essential to address the cause of the injury. This may improve the proprioception around the knee for someone with hypermobility and increase strength and control of the leg and knee with exercises. Additionally, looking at walking or running gait can be very important if this contributes to the onset of pain or if it contributes to recovery.

