The searing back pain came out of nowhere. You crumpled over in agony unable to move. Your doctor thinks you may have injured your disc. What is a herniated disc? How to diagnose a herniated disc? Can a herniated disc heal on its own? What are the treatment options for a herniated disc? How to heal a herniated disc naturally? Let’s dig in.
The spine is compromised of boney building blocks called vertebral bodies. They are numbered and their specific location is noted by one of three letters: Cervical, Thoracic or Lumbar. Sandwiched between the vertebral bodies are shock absorbers called discs. A disc has two principal parts: the jelly-like inside called the nucleus pulposis and the tough outer layer called annulus fibrous(1).
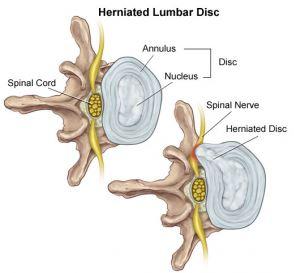
A disc herniation is when the jelly-like inside ruptures through the tough outer wall (2). Think of it like a pimple that has popped. The ruptured material is highly inflammatory and can cause:
- Severe irritation and swelling in the area of the herniated disc (localized pain)
- Place pressure on a spinal nerve causing pain to radiate down the arm or leg (radicular)
A disc herniation is NOT a disc bulge or protrusion as in both in both these conditions the jelly-like material is still contained in the disc. Disc herniation occurs most commonly in the lumbar spine between the fourth and fifth decade of life (3). Factors associated with lumbar disc herniation include genetic predisposition (4), disc degeneration (5), and excessive loading (6).
Lumbar disc herniation is the condition that most often leads to spinal surgery, especially among men around the age of 40 years (7).
How To Diagnosis a Herniated Disc
Magnetic resonance imaging (MRI) is the gold standard for imaging (8). X-ray only demonstrates bone. An x-ray can not identify a disc herniation and it can not visualize any soft tissue such as disc, tendons, or ligaments. If your spine pain is constant and radiating down your arm or leg insist upon an MRI.
Can a Herniated Disc Heal on Its Own?
Despite what a surgeon may advise you the answer is YES. Lumbar discs healing on their own is well documented using MRI (9). The medical term for this is a regression which references a resolution or reduction of the disc herniation. The healing may be partial or complete. The largest obstacle to healing spinal injuries is the poor blood supply. Blood flow is critical to healing as it brings important nutrients and healing proteins to the area of injury.
How and why regression occurs is not fully understood. The three most popular theories:
- The herniated disc becomes dehydrated and shrinks in size (10).
- Tension from the adjacent ligament (PLL) forces the herniated disc back into place (9).
- The herniated disc is absorbed by the body (11).
What Are the Treatment Options for a Herniated Disc?
The specific treatment for a herniated disc will depend upon the extent of the disc herniation, its location, whether or not it is compressing a nerve, and the presence or absence of muscle weakness or numbness in the arm or leg. When appropriate, physical therapy is the first-line treatment. The focus is on mobilization, neutral spinal alignment, and core stabilization.
Supplements
Inflammation can cause significant problems and delay recovery. A recent study looked a 100 patients with low back disc herniations and followed them for one year (12). Those with elevated inflammation markers (IL-6) were approximately 3.5 x less likely to recover that year. A good quality fish oil and Turmeric are safe, effective anti-inflammatory agents. NSAID medications like Motrin, Aleve, and Celebrex are toxic to stem cells, and associated with a higher risk of sudden death heart attack. NSAID’s therefore should be avoided.
Surgery
When conservative therapy fails surgery is often recommended. There are a number of different types of back surgery for disc herniations. All accomplish the same thing which is cutting out the herniated disc. This procedure is called a discectomy. There are different surgical approaches that differ in invasiveness. Open discectomy cuts through the low back muscles and has many different problems including killing off important spinal stabilizing muscles. The newer approaches are ” minimally invasive” and utilize small cameras and instruments. The procedures work the same as far as outcomes and complications, but the minimally invasive procedure has a quicker recovery time (13). Unfortunately for patients, the failure rate of spinal surgery ranges from 10-50% (14-16). This means the patients were classified as having continued low back or leg pain or new disabling symptoms after the surgery which is called Failed Back Surgery Syndrome. To learn how to avoid failed back surgery syndrome please see my previous blog. Given the issues with back surgery for disc herniations, the important question becomes how to heal a herniated disc naturally.
Is There a Natural Way to Treat a Herniated Disc?
In answer to your question about how to heal a herniated disc naturally, Yes! PRP is an effective treatment option for herniated discs. PRP is rich in growth factors that increase blood flow and reduce inflammation. Recall that most structures in the spine have little or poor blood flow. This poor blood flow in turn makes healing and repair difficult. PRP injections can overcome this issue as the growth factors can increase the blood flow to the herniated disc. To learn more about PRP please click on the video below.

Meet JR a patient at the Centeno-Schultz Clinic who had severe low back pain due to low back disc herniation in 2017. He declined surgery and opted to treat his herniated disc naturally and underwent PRP epidural and facet injections. His pain quickly improved and JR went back to all his normal activities within several weeks after the injections. Below his low back MRI images before and after PRP injections.
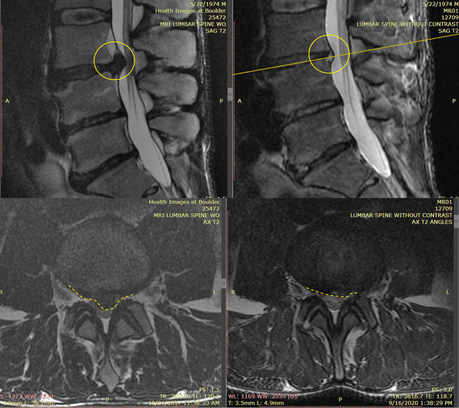
The MRI images on the left are prior to the PRP injection. The top, left image is looking at the patient’s side. The bottom left is called an axial image and is the image if we “saw you in half”. The disc herniation is the dark protruding object circled in yellow. On the top image, the yellow circle is solid whereas in the lower image it is dashed. OUCH! It is no wonder that JR had severe low back pain. The images on the right are 2 years after the PRP injections and resolution of pain. The yellow circle in the top, right image, and the dashed circle in the bottom right image show a significant reduction in size in the disc herniation. This corresponds with the 100% resolution of pain.
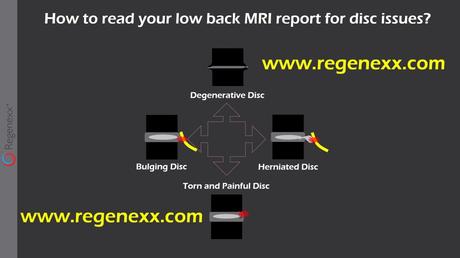
If you have ongoing low back and are interested in learning more about how to read and understand your low back MRI report please click on the video below.
In Conclusion
A disc herniation is when the jelly-like center of the disc ruptures through the tough outer sidewall. Herniations occur most frequently in the low back. They can cause severe localized low back pain or radiating nerve pain down the leg or both. Disc herniations are best diagnosed by an MRI. A herniated disc can heal on its own. Treatment options include conservative therapy and surgery. The failure rate of spinal surgeries ranges from 10-50%. Surgery oftentimes fails and the patient despite the surgery and rehabilitation continues to have pain. This is called failed back surgery syndrome. PRP is an effective non-surgical treatment option. PRP is a way to heal disc herniations naturally without the risk and complications of spinal surgery.
If you have sustained a disc herniation know that you have treatment options. The operating room is not the only solution. Surgeons are biased towards surgical solutions. Schedule a telemedicine consult and learn from a board-certified physician your treatment options.
1.Kos N, Gradisnik L, Velnar T. A Brief Review of the Degenerative Intervertebral Disc Disease. Med Arch. 2019;73(6):421-424. doi:10.5455/medarh.2019.73.421-424
2.Vialle LR, Vialle EN, Suárez Henao JE, Giraldo G. LUMBAR DISC HERNIATION. Rev Bras Ortop. 2015;45(1):17-22. Published 2015 Nov 16. doi:10.1016/S2255-4971(15)30211-1
3.Bortoletto A, Prata SD, Bonfim dos Santos G. Hérnia discal em crianças e adolescentes: relato de cinco casos. Rev Bras Ortop. 1998;33(10):811–814.
4.Janeczko Ł, Janeczko M, Chrzanowski R, Zieliński G. The role of polymorphisms of genes encoding collagen IX and XI in lumbar disc disease. Neurol Neurochir Pol. 2014 Jan-Feb;48(1):60-2. doi: 10.1016/j.pjnns.2013.04.001. Epub 2014 Jan 23. PMID: 24636772.
5. Brayda-Bruno M, Tibiletti M, Ito K, Fairbank J, Galbusera F, Zerbi A, Roberts S, Wachtel E, Merkher Y, Sivan SS. Advances in the diagnosis of degenerated lumbar discs and their possible clinical application. Eur Spine J. 2014 Jun;23 Suppl 3:S315-23. doi: 10.1007/s00586-013-2960-9. Epub 2013 Aug 27. PMID: 23978994.
6.Lotz JC, Chin JR. Intervertebral disc cell death is dependent on the magnitude and duration of spinal loading. Spine (Phila Pa 1976). 2000 Jun 15;25(12):1477-83. doi: 10.1097/00007632-200006150-00005. PMID: 10851095.
7. Spangfort EV. The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand Suppl. 1972;142:1-95. doi: 10.3109/ort.1972.43.suppl-142.01. PMID: 4516334.
8.Kim KY, Kim YT, Lee CS, Kang JS, Kim YJ. Magnetic resonance imaging in the evaluation of the lumbar herniated intervertebral disc. Int Orthop. 1993;17(4):241-4. doi: 10.1007/BF00194188. PMID: 8407042.
9. Teplick JG, Haskin ME. Spontaneous regression of herniated nucleus pulposus. AJR Am J Roentgenol. 1985;145(2):371–5 PubMed PMID: 3875236.
10.Henmi T, Sairyo K, Nakano S, Kanematsu Y, Kajikawa T, Katoh S, et al. Natural history of extruded lumbar intervertebral disc herniation. J Med Investig. 2002;49(1–2):40–3 PubMed PMID: 11901758.
11. Autio RA, Karppinen J, Niinimaki J, Ojala R, Kurunlahti M, Haapea M, et al. Determinants of spontaneous resorption of intervertebral disc herniations. Spine. 2006;31(11):1247–52 PubMed PMID: 16688039.
12. Schistad EI, Espeland A, Pedersen LM, Sandvik L, Gjerstad J, Røe C. Association between baseline IL-6 and 1-year recovery in lumbar radicular pain. Eur J Pain. 2014 Nov;18(10):1394-401. doi: 10.1002/j.1532-2149.2014.502.x. Epub 2014 Apr 2. PMID: 24692238.
13. “Doctors getting rich with fusion surgery debunked by studies:” Bloomberg, Dec 30 2010. Accessed 10/12/19. https://www.bloomberg.com/news/articles/2010-12-30/highest-paid-u-s-doctors-get-rich-with-fusion-surgery-debunked-by-studies.
14. Clancy C, Quinn A, Wilson F. The aetiologies of failed back surgery syndrome: a systematic review. J Back Musculoskelet Rehabil. 2017;30(3):395–402 https://www.ncbi.nlm.nih.gov/pubmed/27689601
15. Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979–987. Published 2016 Nov 7. doi: 10.2147/JPR.S92776.
16. Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Chronic opioid therapy after lumbar fusion surgery for degenerative disc disease in a workers’ compensation setting. Spine (Phila Pa 1976). 2015;40(22):1775–1784 https://www.ncbi.nlm.nih.gov/pubmed/26192725

