 I shouldn't have being playing golf Thursday. I woke that morning feeling lethargic. I had a nagging pain in the middle of my upper back. But with my history of pericarditis, and more recently, arthritis, I seldom go through the week without some pain here or there. I decided to ignore the way I felt and play golf. That was my first mistake.
I shouldn't have being playing golf Thursday. I woke that morning feeling lethargic. I had a nagging pain in the middle of my upper back. But with my history of pericarditis, and more recently, arthritis, I seldom go through the week without some pain here or there. I decided to ignore the way I felt and play golf. That was my first mistake.I took an Ibuprofen, threw my clubs in the car and drove to the course. I was playing with my good friend, who'd invited me to play at his club at Meadow Springs, a beautiful course nested along the Amon Basin creek watershed. The sky was overcast as I parked and checked in. By the time we were standing on the tee, about 12:00, a slight drizzle had started. My friend asked if I wanted to take the golf cart. I told him I wanted to walk the first Nine to get some exercise. That was my second mistake.
Because course maintenance was taking place on the Front Nine, the pro shop started us on No. 10, which is an elevated tee crossing Amon Creek at the bottom of the hill. After that, the course regains altitude at a steep rate. By the time I'd negotiated the first six holes, I was having trouble catching my breath. At the No. 16 tee I had a pressing feeling in my chest. Did I quit? No, I struggled on. That was my third mistake. You know what they say about three strikes.
I finished the round, joined my friend for lunch, which I couldn't finish, and went home. I lay down for an hour, took a shower, and joined my wife on the couch. This was about 5 pm. By this time I was experiencing a severe throbbing pain radiating up my left carotid artery into my neck. I went back and lay down.
My wife came in and asked me what was happening. She said I should go to the emergency room. I said I'd take an aspirin and wait it out. Another mistake.
I couldn't sleep. I tried elevating my head and back, something I'd done when I had pericardial pain. It didn't help much. I continued to have the throbbing pain up my left carotid artery, into my neck, and over to my shoulder. I was sweating. I took 3 more aspire @ 325 mg ea over the next 8 hours.
The next morning, a Friday, March 29th, I called my primary care physician and speaking to the receptionist asked to have an appointment ASAP. She said she could get me in Monday. I said okay. She asked me why I needed the appointment. I said, "I'm having chest pain." She said just a minute. Then she came back on the line and said, "Go to the emergency room." This time I followed instructions.
*********************************************As it turns out, if you're experiencing chest pains, the best advice is to call 911. This way you'll get directly to the ER, you'll get there quickly, and you'll likely get emergency treatment along the way. Going to your primary care physician first is poor policy, if you are having a heart attack. Learn to recognize the symptoms and be smarter about taking action than I was. The longer you delay, the more heart damage you'll have, and the longer your recovery will be -- assuming you recover.
*********************************************My son drove me to the nearest emergency room, which was at Kennewick General Hospital (KGH). When I told the person manning the reception desk my problem, he took me right to the triage nurse; the first time I hadn't been asked for ID and insurance when going to the hospital. I was with the triage nurse for no more than 3 minutes before I was taken to a room and placed on an examining table.
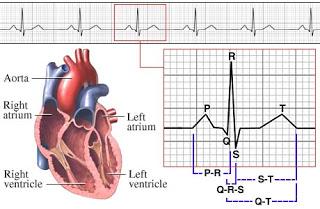
Before I knew it, a lab tech had taken blood, I had an IV in my right arm near the wrist, and had been wired for an ECG. After the ECG a technician wheeled in an X-Ray machine and did a chest X-Ray. At some point, a nitroglycerin patch was placed on my chest. The IV contained a blood thinner, easing the blood pumping burden on my heart.
The attending physician, a Dr. Richard Kinder, came in to see me about 20 minutes into this process. He told me indications were that I'd had a heart attack. KGH didn't have a cardiac specialist available to do a catheterization, so they were transferring me to Kadlec. He asked me who my doctor was, and I told him my cardiologist was Dr. Surrender Wadha. Kinder said he'd notify him.
I was transferred to Kadlec by ambulance. One of the EMTs sat in the back with me and monitored my vital signs. It took 18 minutes to get from KGH to Kadlec. On the way I learned the EMT liked to read and promised him a signed copy of my soon-to-be-published novel, The Lion and the Sun. I was assuming I'd be alive to sign the book when it was published. I'm an optimist.
At Kadlec I was taken directly to the cardio ward, where ECG sensors were attached to my chest and connected to a transmitter that sent signals wirelessly to a display at the side of the bed.

 An IV drip was started, and additional blood work was done. Another ECG was performed. My cardiologist, Dr. Wadhwa, walked into the room a few minutes later. Friday was normally his day off. He'd be in checking on me the next two days, Saturday and Easter Sunday.
An IV drip was started, and additional blood work was done. Another ECG was performed. My cardiologist, Dr. Wadhwa, walked into the room a few minutes later. Friday was normally his day off. He'd be in checking on me the next two days, Saturday and Easter Sunday.Dr. Wadhwa put his stethoscope on my chest and as he listened to my chest he told me that my ECG was abnormal -- I had an inverted t-wave -- and blood work indicated I'd had a myocardial infarction, commonly known as a heart attack. I asked how blood work indicated a heart attack. Dr. Wadhwa told me that my troponin level was elevated.
 The troponin test measures the levels of certain proteins called Troponin T and Troponin I in the blood. These proteins are released when the heart muscle has been damaged, such as a heart attack. The more damage there is to the heart, the greater the amount of Troponin T and I there will be in the blood. An increase in the troponin level, even a slight one, usually means there has been some damage to the heart. Significantly high levels of troponin are a sign that a heart attack has occurred. Cardiac troponin levels are normally so low they cannot be detected with most blood tests. Test results are usually considered normal if the results are between zero and 0.10 ng/mL. My Troponin I was 2.64.Another test that showed evidence of an heart attack was Creatine Kinase-MB (CK-MB). A CK-MB of more than 2.5 to 3 is indicative of heart damage. Mine was 10.7.Wadhwa has been my cardiologist for many years. I saw him regularly because of my history of pericarditis. Even though I'd had my pericardium removed, I had over the years experienced pain of the type I experienced when I had a pericardium. We'd assumed it was from residual pericardial tissue left around major arteries, either that or an unrelated cause, such as arthritis, sprains, congestion, infection, or imagination. Wadhwa knew that I was proficient with the Internet and did a considerable amount of research on medical issues. He had always been very open with me and willing to discuss matters associated with my history of heart problems. I'd even offered to will him my heart after (I was sure to stipulate, after my death) to use in research on long-term survival of pericardectomy survivors (he wasn't interested).Wadhwa told me that he wanted to have coronary angiography performed and said he was trying to contact a doctor that he believed was the best at doing the procedure. I wasn't anxious to have this done, mainly because I didn't like the risk involved in having a wire inserted into my coronary arteries and I wasn't sure the test was required. Wadhwa convinced me otherwise by pointing out my history of high cholesterol and the fact that I'd gone off my cholesterol medication several months previously because of myopathy brought on by the statins in the medications. He said that with the test we could determine if my heart attack had been brought on by clogged arteries or something else. This would help determine the course of therapy. I couldn't argue with the logic.I was wheeled to the "cath lab" around noon Friday. My wife and my son accompanied me as far as the prep room, where my groin area was shaved. An angiogram can be done by inserting the catheter through the femoral artery in the groin (most common), or through the radial artery in the forearm. I had the former procedure. An estimated 3 million coronary angiograms are performed in the United States each year to look for blockages in coronary arteries. The radial artery is currently used in less than 5% of them. However, a recent study suggests angiography using the radial artery is just as effective as the technique using the femoral artery, and patients report finding the procedure less uncomfortable. I did not experience any significant pain during or after the procedure.
The troponin test measures the levels of certain proteins called Troponin T and Troponin I in the blood. These proteins are released when the heart muscle has been damaged, such as a heart attack. The more damage there is to the heart, the greater the amount of Troponin T and I there will be in the blood. An increase in the troponin level, even a slight one, usually means there has been some damage to the heart. Significantly high levels of troponin are a sign that a heart attack has occurred. Cardiac troponin levels are normally so low they cannot be detected with most blood tests. Test results are usually considered normal if the results are between zero and 0.10 ng/mL. My Troponin I was 2.64.Another test that showed evidence of an heart attack was Creatine Kinase-MB (CK-MB). A CK-MB of more than 2.5 to 3 is indicative of heart damage. Mine was 10.7.Wadhwa has been my cardiologist for many years. I saw him regularly because of my history of pericarditis. Even though I'd had my pericardium removed, I had over the years experienced pain of the type I experienced when I had a pericardium. We'd assumed it was from residual pericardial tissue left around major arteries, either that or an unrelated cause, such as arthritis, sprains, congestion, infection, or imagination. Wadhwa knew that I was proficient with the Internet and did a considerable amount of research on medical issues. He had always been very open with me and willing to discuss matters associated with my history of heart problems. I'd even offered to will him my heart after (I was sure to stipulate, after my death) to use in research on long-term survival of pericardectomy survivors (he wasn't interested).Wadhwa told me that he wanted to have coronary angiography performed and said he was trying to contact a doctor that he believed was the best at doing the procedure. I wasn't anxious to have this done, mainly because I didn't like the risk involved in having a wire inserted into my coronary arteries and I wasn't sure the test was required. Wadhwa convinced me otherwise by pointing out my history of high cholesterol and the fact that I'd gone off my cholesterol medication several months previously because of myopathy brought on by the statins in the medications. He said that with the test we could determine if my heart attack had been brought on by clogged arteries or something else. This would help determine the course of therapy. I couldn't argue with the logic.I was wheeled to the "cath lab" around noon Friday. My wife and my son accompanied me as far as the prep room, where my groin area was shaved. An angiogram can be done by inserting the catheter through the femoral artery in the groin (most common), or through the radial artery in the forearm. I had the former procedure. An estimated 3 million coronary angiograms are performed in the United States each year to look for blockages in coronary arteries. The radial artery is currently used in less than 5% of them. However, a recent study suggests angiography using the radial artery is just as effective as the technique using the femoral artery, and patients report finding the procedure less uncomfortable. I did not experience any significant pain during or after the procedure.
Cath Lab
During coronary angiography, special dye is released into the bloodstream. The dye makes the coronary arteries visible on x-ray pictures. This helps doctors see blockages in the arteries. Cardiac catheterization is used to get the dye into the coronary arteries. For this procedure, a thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream. X-ray pictures are taken while the dye is flowing through the coronary arteries.Dr. Iyad Jamali performed my procedure. He came to the side of the operating table and introduced himself. Jamali went to medical school at the University of Damascus, in Syria, and was struck by my resemblance to a colleague of his. He described the procedure for me, and kept me informed throughout it. A nurse applied local anesthetic (1% lidocaine) to my right groin. Jamali said, "You're going to feel a slight pinch," and inserted the arterial sheath through which he'd thread the catheter. My wife told me later that the procedure took twenty minutes. I was awake throughout. Afterward, Jamali came out and told us that my coronary arteries were clear. Jamali also told us that I had a significant gradient between the apical segment and mid segment of the left ventricle. He thought this likely due to segmental hypertrophy cardiomyopathy. Jamali thought it advisable that I undergo a cardiac MRI and OTE. Hypertrophic cardiomyopathy (HCM) is a genetic cardiac disease that can cause sudden death, or go undetected for the affected person's lifetime. Unless my lifetime is 75 years, I fall into the latter group.
Prior to my release from the hospital on a bright, sunny Easter morning, I underwent an Echocardiogram. According to Dr. Wadhwa, the results were little different that many previous echos I had in his office. My instructions from Wadhwa were to go home and take it easy. He put me on Coregto slow my heart and allow it to heal, and Ibuprofen twice a day for pain. He said my recovery would take 6 to 8 weeks. I was to see him on May 10th.
One week after my release from the hospital, I'm essentially free of pain, I have no shortness of breath, or dizziness, and I'm going stir crazy.

