Cervical Spine Instability Measurements: How To Precisely Interpret Them
It was all a blur. You were waiting for the red light to change when a large truck slammed into your vehicle. You did not see the approaching vehicle but heard the skidding tires. The brain fog, dizziness and fatigue have not responeded to conservative therapy. Work and domestic responsibilites are overwhelming and difficult to complete. Isolation and sadness are constant companions. Your surgical consultation was overwhelming. They reviewed the x-rays and MRIs taking different measuresurements. You are so confused. What are cervical spine instability measurements? What are the basic structures in the cervical spine?
Introduction
Injuries to the upper cervical spine can cause a large number of poorly recognized or understood symptoms such as brain fog, dizziness and severe fatigue. As such many such injuries are misdiagnosed or missed altogether. Many patients are inappropriated labeled as psychologically unstable or hormonal. Cervical spine instability is real and can profoundly affect patients and their families alike. Cervical spine instability measurements are important to understand as they can lead to the accurate diagnosis of injuries to the upper cervical spine.
The Spinal Anatomy: An Overview
To understand Cervical Spine Instability Measurements, a basic review of neck anatomy is in order. The Cervcial Spine is composed of Discs, Facet joints, ligaments, nerves, tendons and tendons.
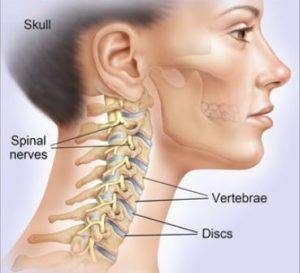
Bones
The bones in the neck are stacked upon one another. They are also known as vertebral bodies. These boney building blocks are numbered 1 through 7. The letter C precedes each number indicating that we are referencing the Cervical Spine. C=cervical. The top bone is the C1 and is also referred to as the Atlas. The lowest bone in the neck is the C7
Discs
The Disc is a fibrocartilage cushion that is sandwiched between each of the Vertebral Bodies. It is an important shock absorber. Its name is based on the bones it is sandwiched between. For example, the Disc between the C6 and C7 Vertebral Body is referred to as the C6/7 disc. It is susceptible to injury. Common examples of Disc injuries include Protrusions, Herniations, and Extrusions.
Facet Joints
The Facet Joints are small, paired joints on the backside of the neck. There is right and left Facet Joint at each spinal level. The Facet Joints provide important stability to the neck and limit movement. Like the knee and ankle joints, the Facet Joints are lined with cartilage which allows for smooth, pain-free motion. Unfortunately, Cervical Facets is susceptible to injury with the compromise of the joint cartilage and joint health. The result can be a limited range of motion in the neck and pain.
Ligaments
Ligaments are thick pieces of connective tissue that connect bone to bone. Essentially they are human Duck tape. They provide stability for the neck and head. There are a large number of ligaments in the Cervical Spine. The two most important ligaments are the Alar and Transverse ligaments. These ligaments essentially connect your head to your neck. Unfortunately, these ligaments are susceptible to injury.
Tendons
Tendons are connective tissue that connect muscle to bone. Muscles and tendons in the Cervical Spine provide important stability and enable movement. Tendons are susceptible to injury due to trauma, repetitive use, and degeneration. Injured tendons can jeopardize neck stability, health, and movement. The consequences can be nech pain, headaches, and a limited range of motion.
Spinal Cord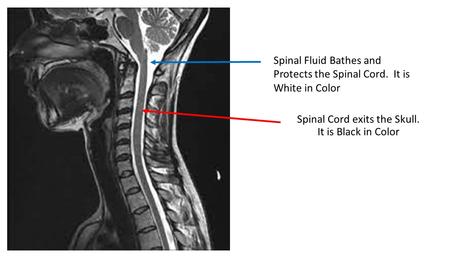
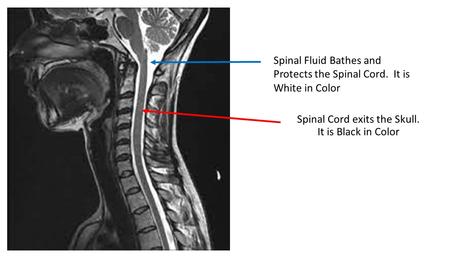
The Spinal Cord consists of neural tissue that starts at the base of the brain and extends down into the low back. It is a cylindrical bundle of nerve fibers that control our voluntary and involuntary bodily functions. It carries signals between the brain and the rest of the body. As the Spinal Cord descends from the skull and through the neck and rest of the body it is protected on all sides by spinal bones. These bones provide a boney armor to protect against injury. The Spinal Cord has an additional layer of protection afforded by the spinal fluid. The spinal fluid is also known as Cerebral Spinal Fluid. It surrounds the Spinal Cord and extends the entire length of the spine. The image to the right is a side view of the Spinal Cord as it exits the brain. The Spinal Cord is black in color. The white that surrounds it is the spinal fluid.
Cranial NervesAs the Spinal Cord descends through the Foramen Magnum and spine, important nerves branch off traveling to different parts of the body. There are a large number of nerves. These include the 12 Cranial nerves some of which control muscles whereas others are connected to internal organs such as the heart and lungs.
Arteries and Veins
Arteries and veins provide blood flow to and from important structures in the head, neck, and body. Without blood flow, the body can not function.
What Is the Alar Ligament? 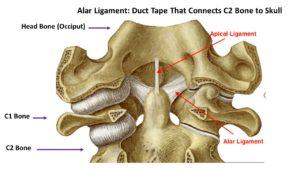
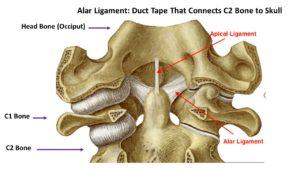
Ligaments are thick bands of connective tissue that connect one bone to another. The Alar ligament is a critical ligament in the upper neck as it connects your head to your neck. It connects the C2 bone (Dens) to the base of the skull. There is a right and left Alar ligament. Injury to the Alar ligament can lead to Craniocervical Instability. To learn more about this condition, its symptms and nonsurgical treatment options please click here.
What Is the Transverse Ligament? 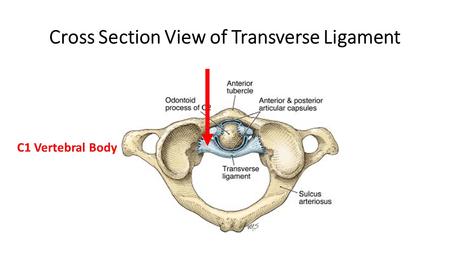
The Transverse ligament is a thick band of connective tissue that snuggly holds the C2 bone in place. Like the Alar ligament it provides important stability in the upper neck. To learn more about the Transverse ligament please click here.
Cervical Spine Instability
Stability is important for optimal function. Take the wheels on your vehicle for example. Properly adjusted lug nuts allow your wheel/ tires to perform optimally. This in turns allows your car to travel at appropriate speeds in a wide range of conditions including rain and snow. If however the lug nuts are loose, the wheel is unstable which severely compromises your ability to travel at any speed, or any distance.
So too with Cervical Spine. Optimal neck function requires that the Cervical Discs, Facet Joints, and ligaments are stable and in proper alignment. Stability is dependent upon muscle strength and ligament integrity. Injury or laxity of the neck ligaments can lead to compromise Cervical Spine stability and optimal function. Instability puts the neck Discs, Facet joints and nerves are risk for injury resulting in pain, impaired function, and restriction in range of motion.
Types Of Cervical Spine Instability
There are many different types of Cervical Instability. Symptoms vary depending upon the severity of the instability. The two major types of Cervical Instability are:
Craniocervical Instability (CCI)
Craniocervical Instability involves the ligaments that hold your head onto your neck (1). The principal ligaments are the Alar and Transverse ligaments. When these ligaments become injured or loose there is excessive motion of the head on the neck. This in turn can cause a constellation of debilitating symptoms. To learn more about CCI and nonsurgical treatment options please click here.
Atlantoaxial Instability (AAI)
The Atlas is the C1 bone. The Axis is the C2 bone. The C1 and C2 bone come together and form a joint that is appropriately called the Atlantoaxial joint (AA). When supporting ligaments are injured or become loose the joint becomes unstable resulting in pain and functional decline (2). To learn more about the Atlantoaxial joint please click here.
Why Measurements Are Necessary
Cervical Spinal Instability Measurements are important as they can help establish the diagnosis of Cervical Instability. This diagnosis is poorly recognized or understood by most physicians. Symptoms can vary signficantly from patient to patient. Futhermore most Cervical Spine MRIs do not examine or report on the integreity of the Alar, Transverse ligament , C0/1, C1/2 joints. At the Centeno-Schultz Clinic we manually calculate a patient’s Cervical Spine Instability measurements.
How Is Cervical Instability Measured? (Static vs Dynamic Measurements)
One of the most confusing things for patients to appreciate is that Cervical Instability is a dynamic concept which by definition involves motion. In medicine, for something to be “unstable” means that is moves more than it was designed to. This excessive motion can cause signficant irritation, injury to key structures like the Spinal Cord, Spinal nerves and joints. Often this can give rise to a variety of symptoms like brain fog, memory problems, fatigue, dizziness and headachess.
Traditonal MRIs are taken with patient lying stationary in a tube. There is no movement so this is a static radiographic study. This unfortunatley is the standard of care of big university medical centers. What is necessary are dynamic tests that can evaluate the cervical spine during motion. Let’s take a deeper look into both static and dynamic measurements
Static Measurements
Grabb-Oakes
The Grabb-Oakes is radiographic measurement used to evaluate upper Cervical Spine conditions. Its measurement involves a two step process. First a line is drawn from the anterior aspect of the Foramen Magnum ( basion) that extends to the inferior backside of the C2 bone (Dens). A second line is then drawn that is peripendicular to this line that extends to the Dura. Given that the C2 bone is held snuggly by the Transverse ligament, a high Grabb-Oakes measurement can be due to a damaged or loose Transverse ligament. An abnormal measurement is often considered to be 9mm or more (3). With the advent of flexion-extension MRI, it’s easier to measure the G-O measurement when the patient moves, which provides more information. To learn more about Grabb-Oakes measurement please click on video below.
Clivo-Axial Angle
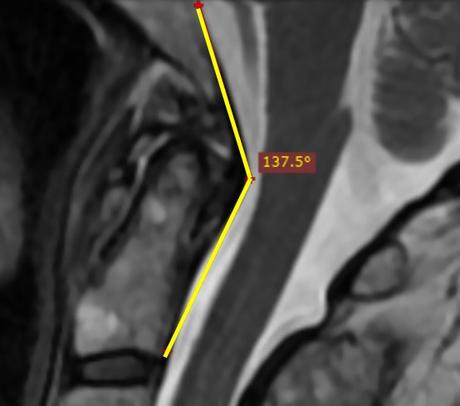
This is the angle between the Clivus and the backside of the C2 bone (Dens) . The problem being measured here is the skull is falling forward on the upper neck which can cause irritation of the front the Brainstem and upper Spinal Cord. This movement is controlled by strong ligaments in the back of the neck at the Nuchal, Supraspinous, and Interspinous ligaments. It’s also controlled by the posterior Atlantoaxial membrane (PAOM, a ligament at the back of the spinal canal) and to a lesser extent the Transverse ligament. Normal and abnormal values vary depending upon the author. Less than 150 degrees (4) was originally reported with others stating that normal is between 145° to 160° in the neutral position (5).
Powers Ratio
This is another measurement that determines if the head has moved forward on the upper neck. This one is more complex, requiring two lines (one between the basion and the back of the spinal canal at C1 and another between the Opisthion and the posterior aspect the front of the Atlas) and then some division is applied. If it’s less than 1, the ratio is normal, if it’s >1 then it’s abnormal. To learn more, see the video below:
Atlantodens Interval (ADI)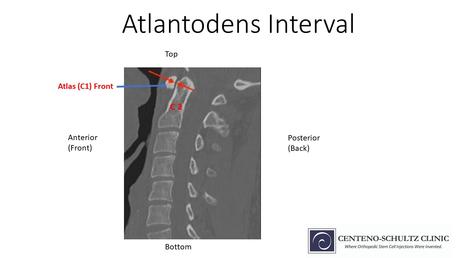
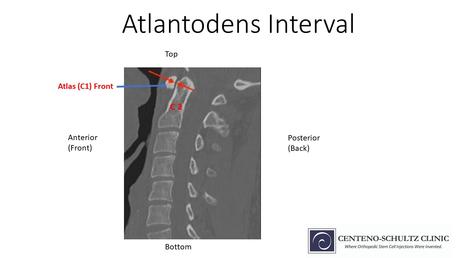
This is the distance between the backside of the C1 bone (Atlas) and the anterior aspect of the C2 bone (Dens). It measures the integrity of the Transverse ligament. Normal value is less than 3mm in adults (6). To learn more about Atlantodental Interval please click here
Movement -Based Measurements (DMX & Upright MRI)
For patients with Cervical Spine Instability it’s critical to understand the differences between static and moving studies. Since instability is a movement-based concept, images that capture what happens to the Craniocervical Junction when it moves will always be far superior to static images. However, because this field is newer, these measurements are less established and the data about what’s normal and abnormal is still being collected
DMX
DMX stands for Digital Motion X-ray, which is an x-ray that is recorded while the patient moves. The patient is put through various manuevers such as bending forward, backwards and to the right and left side. The alignment of the upper Cervical bones is analyzed as the patient is put through various manuevers. The doctor can see the relationship between the bones and when they get out of position with motion, the ligaments holding them are likely injured or stretched out.
The two measurements that upper Cervical Spine Instability patients should pay attention to here are C1-C2 overhang and the ADI. C1-C2 overhang is the amount of motion that happens side to side between the C1 and C2 bone when the patient bends their head to the side (7). This is controlled mostly by the Alar and Transverse ligaments. The ADI stands for Atlantodental Interval and is the distance between the backside of the C1 bone and the front of the C2 bone. In patients with Craniocervial Instability this measurement can increase when they bend forward. To learn more about both measurements, see the video below:
Upright MRI
Traditonal MRIs are static in nature as the patient is lying still on their back. This does not capture motion based problems such as Craniocervical and Atlantoaxial Instability. Upright MRIs however are dynamic in nature as the patient is upright and can be flexed forward or extended backwards. This is a very powerful tool in the evaluation of Cervical Instability. The Grabb-Oakes, Clivoaxial angle and Power’s ratio can be measured in the neutral, forward flexed and extended position. To better understand how this works please watch the video below.
How Proper Diagnosis Can Impact Treatments
Cervical Spine Instability measurements are powerful tools as they can help establish the diagnosis of Upper Cervical Instability. In addition, they can identify the specific ligament or ligaments that are injured or loose. This is critical as it will identify the exact targets that need to be injected under x-ray. The precise injections are with PRP or Bone Marrow Concentrate which contains stem cells.
For example, if a patient has an abnormal Grabb-Oakes measurement, it means that the Transverse Ligament is loose or injured. The Transverse ligament would then be one of the targeted structures in their treatment.
If the Clivio-Axial angle is abnormal the means that the ligaments in the back of the head are loose. Accordingly the Nuchal ligament, Supra and Infraspinous ligaments and PAOM would be targeted structures in their treatment.
If the C1/2 overhang on DMX is abnormal the targeted structures for treatment would be the Alar and Transverse ligament.
Diagnosing Cervical Spine Conditions Needs Precision
One of the most common problems we see in clinic is that patients do not have a formal diagnosis. Neck pain is not a diagnosis but rather is a symptom. It is only when an accurate diagnosis is established that an appropriate treatment plan can be discussed. Too many patients have undergone countless MRIs all of which are normal. This is because they are static imaging with the patient lying down. Dynamic studies such as upright MRI and DMX allow for the evaluation of instability. Cervical Spine Instability measurements are powerful tools that can help in the diagnosis of Upper Cervical Instability.
In Summary
- Cervical Instability is real and regrettably often not appreciated or misdiagnosed.
- Cervical Spinal Instability measurements are important as they can help establish the diagnosis of Cervical Instability.
- The Cervical Spine is composed of bones, discs, facet joints, nerves, arteries, spinal cord and ligaments.
- The Alar and Transverse ligament are the key stabilizer in the Upper Cervical Spine.
- The two most common types of Cervical Spine Instability are Craniocervical Instability (CCI) and Atlantoaxial Instability (AAI).
- Cervical Instability can be evaluated with both static and dynamic measurements.
- Static measurements included the Grabb-Oakes, Clivo-Axial Angle and Atlantodental Interval (ADI).
- Dynamic studies include Digital Motion X-Ray and Upright MRI.
- Cervical Spine Instability measurements can identify specific ligament injuries that can targeted during treatment.
- Neck pain is not a diagnosis. Patients need an accurate diagnosis. Cervical Spine Instability measurements can help in establishing a diagnosis.
If you or a loved one continues to suffer with ongoing brain fog, headaches and dizziness that has not responded to conservative care please schedule a telemedicine consultation. Learn why the countless MRIs have all been read as “normal”. Stop the suffering now.
——————————-
1.Young RM, Sherman JH, Wind JJ, Litvack Z, O’Brien J. Treatment of craniocervical instability using a posterior-only approach: report of 3 cases. J Neurosurg Spine. 2014 Aug;21(2):239-48. doi: 10.3171/2014.3.SPINE13684. Epub 2014 May 2. PMID: 24785968.
2.Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014;4(3):197-210. doi:10.1055/s-0034-1376371
3.Grabb PA1, Mapstone TB, Oakes WJ. Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery. 1999 Mar;44(3):520-7; discussion 527-8. https://www.ncbi.nlm.nih.gov/pubmed/10069589.
4. Khanna G, Sato Y. Imaging of the craniovertebral junction. Oper Tech Neurosurg. 2005;8(3):131–142. doi: 10.1053/j.otns.2005.10.004.
5.Henderson FC Sr, Henderson FC Jr, Wilson WA 4th, Mark AS, Koby M. Utility of the clivo-axial angle in assessing brainstem deformity: pilot study and literature review. Neurosurg Rev. 2018;41(1):149–163. doi:10.1007/s10143-017-0830-3.
6. ADI
7.Radcliff KE et al. Does C1 fracture displacement correlate with transverse ligament integrity? Orthop Surg 2013;5(2):94-9. https://www.ncbi.nlm.nih.gov/pubmed/23658043

