Post-concussion syndrome (PCS) can be a frustrating and debilitating condition for those recovering from a head injury. While most people recover from concussions within a few weeks, some continue to experience lingering symptoms that interfere with daily life. These may include headaches, memory problems, dizziness, and emotional disturbances. Accurately diagnosing PCS is crucial, but it can be complex due to symptom overlap with other conditions. This post will explore what PCS is, what causes it, and how medical professionals test for and diagnose the syndrome.
An Overview Of Post-Concussion Syndrome (PCS)
Post-concussion syndrome is a condition in which symptoms persist beyond the expected recovery period following a concussion, typically lasting weeks to several months or more. These symptoms are not necessarily linked to the severity of the original injury, and they can significantly affect a person’s quality of life.
PCS is characterized by a range of cognitive, emotional, and physical symptoms, such as:
- Persistent headaches
- Difficulty concentrating or remembering things
- Fatigue
- Irritability or mood changes
- Sleep disturbances
- Dizziness or balance issues
Key risk factors that may contribute to the development or persistence of PCS symptoms include:
- A history of previous concussions
- Pre-existing mental health conditions like anxiety or depression
- Younger age or older adulthood
- Female gender (as some studies suggest women may experience symptoms more intensely or for longer durations)
- Lack of proper rest or premature return to physical/mental activity after the injury
Clinical Guidelines For Diagnosing Post-Concussion Syndrome
Diagnosing PCS requires a thoughtful and comprehensive clinical approach. Unlike many conditions that can be confirmed with lab tests or scans, PCS diagnosis is primarily based on patient history and reported symptoms. Several medical organizations, including the American Academy of Neurology (AAN) and the World Health Organization (WHO), have established guidelines for identifying PCS.
Healthcare professionals typically use the following criteria and steps:
- Symptom Duration and Type: PCS is suspected when concussion symptoms persist for more than four weeks in adults and longer in children or adolescents.
- Symptom Clustering: Physicians assess whether multiple symptoms are present across different categories (cognitive, physical, emotional).
- Exclusion of Other Causes: It’s essential to rule out other conditions like migraines, depression, or post-traumatic stress disorder (PTSD), which can mimic PCS symptoms.
Why Recognizing The Symptoms Is The First Step In Diagnosing PCS
Accurate diagnosis of post-concussion syndrome (PCS) begins with a clear understanding and recognition of its symptoms. Since PCS doesn’t show up on routine brain scans and lacks a single definitive test, healthcare providers rely heavily on the patient’s symptom report and medical history to guide diagnosis and management. Recognizing the specific symptoms helps differentiate PCS from other conditions and allows for earlier intervention and targeted treatment.
The challenge, however, is that PCS symptoms can be highly variable, fluctuating in intensity and duration. Moreover, many symptoms overlap with other medical or psychological conditions, such as migraines, depression, anxiety, or even chronic fatigue syndrome.
In fact, some symptoms attributed to PCS, such as dizziness, visual disturbances, and headaches, may originate not from the brain, but from mechanical instability in the cervical spine, particularly the cranio-cervical junction. Recognizing this distinction is essential for accurate diagnosis and effective treatment.
Below is a breakdown of the most commonly reported symptoms of PCS and what they might indicate:
Headaches And Migraines
Headaches are among the most frequent symptoms of PCS. They may resemble tension headaches or migraines and can occur daily. For some, the headaches may worsen with physical or mental exertion, bright lights, or loud noises. In many cases, these headaches are cervicogenic, stemming from dysfunction or ligament injury in the upper neck. They can be extremely uncomfortable and can significantly affect your concentration, making proper identification key for symptom management.
Neck Pain And Dizziness
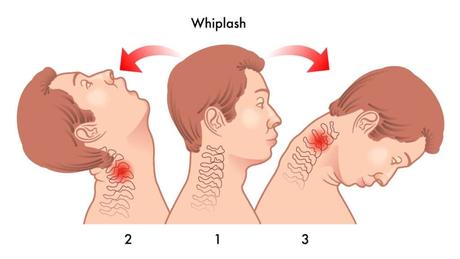
Whiplash or neck strain often accompanies concussions, contributing to ongoing neck pain and dizziness. Dizziness can also result from vestibular dysfunction or visual disturbances related to the brain injury. However, dysfunction in the upper cervical spine, especially at the C0–C2 level, is a major but often overlooked contributor to post-concussion symptoms. Instability or ligament injury in this region can disrupt balance, blood flow, and neural feedback, leading to persistent dizziness, visual disturbances, and headaches that are mistakenly attributed only to brain injury.
Sensitivity To Light And Noise
Photophobia (sensitivity to light) and phonophobia (sensitivity to sound) are hallmark symptoms of PCS. Even mild exposure to bright lights, screen time, or everyday noise can provoke discomfort or headaches. These sensitivities are often overlooked but can be incredibly disruptive, especially in work or school environments.
Fatigue
Fatigue in PCS is not just physical tiredness—it can be mental exhaustion as well. This profound, ongoing fatigue may not improve with rest and can hinder a person’s ability to participate in normal daily activities, especially when coupled with sleep disturbances or cognitive strain.
Brain Fog And Difficulty Concentrating
Described as a feeling of mental cloudiness, “brain fog” is a common cognitive complaint. Individuals may struggle to follow conversations, complete tasks, or stay focused for extended periods. This symptom can be frustrating and often misunderstood, even by the person experiencing it.
In some cases, brain fog may be linked to craniocervical instability (CCI), a condition where loosened ligaments at the junction between the skull and upper cervical spine (C0–C2) impair neural communication and blood flow to the brain. When left undiagnosed, CCI can quietly prolong cognitive symptoms like mental fatigue, slow thinking, and difficulty concentrating.
Memory Issues
Short-term memory lapses, such as forgetting recent conversations, appointments, or tasks, are often reported in PCS. While long-term memory is usually preserved, difficulties with recall can impact confidence and performance at work or school.
Slower Processing Speed
Many people with PCS find that they can still think clearly, but much more slowly. Tasks that once felt automatic may take longer to complete, leading to feelings of inefficiency or mental fatigue. This symptom can affect everything from reading to problem-solving to decision-making.
Anxiety And Depression
Emotional symptoms can arise as a direct result of the brain injury or as a response to dealing with lingering physical and cognitive issues. Anxiety may present as excessive worry or nervousness, while depression might manifest as sadness, hopelessness, or disinterest in activities. These conditions often require parallel treatment along with PCS management.
Mood Swings
Fluctuating emotions—from sadness to irritability to unexpected crying or laughter—are not uncommon. These mood swings may be directly related to brain function changes post-concussion and can also stem from the stress of dealing with ongoing symptoms.
Irritability And Frustration
People suffering from PCS often report feeling “on edge” or having a short fuse. This can be tied to physical discomfort, cognitive strain, or emotional stress. Frustration may also stem from not being understood by others or feeling pressure to return to normal before they are ready.
Insomnia Or Excessive Sleep
Sleep disturbances are common. Some individuals may find it hard to fall asleep or wake frequently throughout the night (insomnia), while others may sleep much longer than usual and still feel unrefreshed. These disruptions can intensify other PCS symptoms, particularly fatigue and cognitive issues.
Trouble Falling Or Staying Asleep
In addition to full-blown insomnia, many patients report taking longer to fall asleep or waking up too early. Poor sleep hygiene, pain, or anxiety can contribute to these patterns, creating a vicious cycle that exacerbates fatigue and emotional symptoms.
Can Medical History Help Diagnose Post-Concussion Syndrome?
A thorough medical history is one of the most valuable tools a physician has when evaluating for post-concussion syndrome (PCS). Since there is no single definitive test for diagnosing PCS, clinicians rely heavily on patient-reported symptoms and a detailed history of the injury event, prior concussions, pre-existing mental health conditions, and any underlying neurological or vestibular issues.
Importantly, a careful review of a patient’s medical background helps rule out other potential causes of symptoms, such as migraines, anxiety disorders, chronic pain syndromes, or even medication side effects. This process of elimination is critical, as many conditions can mimic the cognitive, physical, and emotional symptoms of PCS. The timeline of symptom onset and progression also gives key clues about whether someone is dealing with prolonged concussion effects versus a separate issue.
How Physicians Assess PCS Symptoms Through Clinical Testing
Once a concussion is suspected and symptoms persist beyond the normal healing window, physicians often use a combination of clinical assessments to evaluate the severity and scope of PCS. These include structured symptom inventories, balance testing, eye movement exams, and neurocognitive testing.
The most commonly used clinical tools may include:
- SCAT5 (Sport Concussion Assessment Tool 5th Edition)
- Vestibular/Ocular Motor Screening (VOMS)
- Balance Error Scoring System (BESS)
- Neuropsychological evaluations
Each of these tools is designed to probe different systems potentially affected by a concussion, including balance, coordination, vision, memory, and processing speed.
Vestibular And Cognitive Assessments
Vestibular dysfunction is one of the more under-recognized contributors to PCS symptoms like dizziness, unsteadiness, and spatial disorientation. A study published in the Journal of Neurotrauma found that nearly 60% of patients with prolonged concussion symptoms demonstrated vestibular impairments. Tests like the VOMS are used to evaluate eye movements, head movement tolerance, and balance—key areas often disrupted after a head injury.
Cognitive assessments, such as memory recall tasks and attention span evaluations, help identify deficits in executive functioning. These are especially important when patients complain of “brain fog” or difficulty concentrating.
Neurocognitive Testing
Computerized neurocognitive tests, like ImPACT or CNS Vital Signs, measure functions like attention, processing speed, verbal memory, and reaction time. According to a review in the British Journal of Sports Medicine, these tools can aid in understanding the extent of brain dysfunction, especially when tracked over time. They are often used alongside symptom inventories to create a more complete picture of a patient’s cognitive recovery trajectory.
SCAT5 (Sport Concussion Assessment Tool 5th Edition)
The Sport Concussion Assessment Tool – 5th Edition (SCAT5) is a widely used, standardized tool designed to evaluate individuals suspected of having a concussion, particularly in sports-related settings. Endorsed by the International Consensus on Concussion in Sport, SCAT5 is suitable for use by trained healthcare providers and can be applied on the sidelines or in clinical environments. It offers a comprehensive, multi-part assessment that examines a patient’s symptom profile, cognitive functioning, and neurological status. The tool includes a symptom checklist where individuals rate the severity of 22 symptoms such as headache, dizziness, and difficulty concentrating. It also incorporates cognitive screening through orientation questions, immediate and delayed memory recall, and concentration tasks like digit span and reciting the months of the year in reverse.
Additionally, SCAT5 includes a brief neurological exam that assesses coordination and balance, and it starts with the Glasgow Coma Scale (GCS) to determine the level of consciousness. For athletes, the tool includes Maddock’s questions—brief orientation queries to quickly evaluate mental status following injury. Although SCAT5 is a valuable aid in concussion assessment, it is not intended to diagnose a concussion on its own but rather to support clinical judgment with structured observations.
Balance Error Scoring System (BESS)
The Balance Error Scoring System (BESS) is another key tool used to assess postural stability following a concussion. It is a simple, cost-effective method for detecting balance impairments that often accompany head injuries. BESS evaluates a person’s ability to maintain balance in three different stances—double-leg, single-leg, and tandem—performed on both firm and foam surfaces. Each stance is held for 20 seconds with eyes closed and hands placed on the hips, while a healthcare provider records the number of balance “errors” such as opening the eyes, stepping, stumbling, or lifting the hands off the hips. The total error count helps determine the level of postural instability, with a higher number of errors indicating greater impairment.
BESS is particularly useful during the early stages after a concussion and can be repeated over time to track recovery. Often used alongside SCAT5 or vestibular assessments, BESS provides insight into how the concussion has affected the body’s balance and coordination systems, making it a valuable component of the broader clinical evaluation process.
When Are Imaging Options Needed?

While PCS is primarily diagnosed through clinical evaluation, imaging studies can play a role in ruling out more serious structural injuries. Physicians may order a CT scan or MRI if symptoms are severe, progressively worsening, or associated with “red flag” warning signs like:
- Seizures
- Loss of consciousness
- Severe headaches
- Vomiting
- Neurological deficits (e.g., numbness, vision changes)
However, it’s important to note that routine imaging often appears normal in PCS cases, because standard CT and MRI scans cannot detect the subtle functional disruptions that cause PCS symptoms. This is why imaging is reserved for specific cases and is not used to confirm PCS on its own.
Standard CT and MRI are not designed to capture motion-dependent cervical spine instability, particularly in the atlantoaxial region. This is why patients with persistent symptoms but normal imaging may still have undiagnosed issues stemming from the neck.
The Importance Of Getting Your Neck Checked
One frequently overlooked contributor to prolonged PCS symptoms is cervical spine injury. A concussion is often accompanied by whiplash-like forces to the neck, particularly in motor vehicle accidents or sports injuries. If these cervical injuries go undiagnosed, they can manifest as headaches, dizziness, neck pain, and even visual disturbances—symptoms that overlap heavily with PCS.
Instability in the cervical spine region can lead to brainstem compression, altered CSF flow, and autonomic dysfunction. Conditions that mimic or worsen PCS. According to a study in the Journal of Orthopaedic & Sports Physical Therapy, treating cervical spine dysfunction can significantly reduce symptoms previously attributed solely to PCS. Issues such as joint instability, muscle tension, or restricted range of motion may prolong the recovery process if left unaddressed.
This sets the stage for a more advanced diagnostic option: Digital Motion X-Ray, which can help detect cervical spine problems that static imaging might miss.
Digital Motion X-Ray In Post-Concussion Evaluation
Digital Motion X-Ray (DMX) is a specialized imaging technique that captures real-time motion of the cervical spine using high-speed X-ray video. Unlike traditional MRI or CT scans, which take static images, DMX records the neck and upper spine while the patient moves—allowing physicians to observe dynamic instabilities or abnormal movement patterns.
This is especially useful in PCS patients who have persistent symptoms like:
- Headaches
- Dizziness or vertigo
- Neck stiffness
- Jaw pain
- Balance issues
DMX can reveal subtle ligamentous injuries, joint misalignments, or vertebral instability that are commonly missed on standard imaging. This makes it a valuable tool in a comprehensive PCS evaluation, especially when neck trauma is suspected.
Your Recovery Starts With An Accurate Diagnosis
The key to effective PCS treatment is an accurate, thorough diagnosis. Since symptoms can be broad and multifaceted, a personalized evaluation, factoring in medical history, clinical testing, cognitive assessments, and advanced imaging when necessary, is essential.
Recognizing and addressing all contributing factors, including neck injuries, vestibular dysfunction, and emotional health, can significantly improve outcomes and reduce recovery time. If you or someone you love is dealing with lingering symptoms after a concussion, don’t wait—early evaluation leads to better recovery.
Lingering concussion symptoms? Contact Centeno-Schultz Clinic today to better understand what might be affecting your recovery.

