Post-concussion syndrome (PCS) is a complex condition that occurs when concussion symptoms persist beyond the expected recovery period. These may include headaches, cognitive difficulties, and emotional instability. Living with post-concussion syndrome comes with unique challenges. You may find that symptoms disrupt aspects of your life, including your ability to work, focus, and manage stress.
While the direct cause of PCS is often a concussion, there can be contributing factors that are less obvious and often misdiagnosed. For example, at the Centeno-Schultz Clinic, our physicians can identify upper neck issues using advanced diagnostic techniques like Digital Motion X-ray (DMX) and upright MRI that cause PCS. An accurate diagnosis is essential to guide informed treatment decisions.
What Is Post-Concussion Syndrome?
A concussion is a mild traumatic brain injury (TBI) that occurs when an impact causes the brain to move quickly and forcefully within the skull.
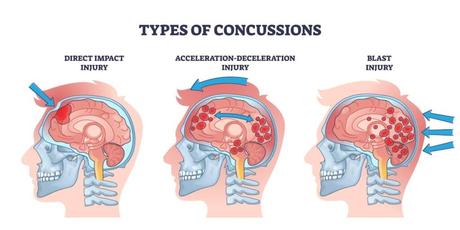
The reactions that occur during a concussion can temporarily disrupt brain function. These include:
- Chemical imbalances: Damage to brain tissues can alter the release of chemicals like neurotransmitters, disrupting the brain’s signaling processes.
- Axonal shearing: Rapid brain movements can stretch or damage tissues and nerve fibers. This can disrupt communication between cells, affecting the processing of nerve signals.
- Inflammation: The body’s response to injury involves inflammation, leading to blood flow increase, pain, and swelling in the brain.
These reactions can lead to a range of symptoms, including headaches, dizziness, confusion, and cognitive difficulties.
Typically, recovering from a concussion involves rest and a gradual return to normal activities. Around 90% of concussion symptoms resolve within 10-14 days. However, sometimes, improper healing and other complications affecting the head or upper neck can cause symptoms to persist. In particular, mechanical dysfunction or instability in the upper cervical spine (C0-C2) can interfere with neural feedback, blood flow, and cerebrospinal fluid dynamics, significantly contributing to lingering symptoms.
You may be diagnosed with post-concussion syndrome (PCS) if you experience the following symptoms for longer than three weeks:
- Headache
- Fatigue
- Dizziness
- Irritability
- Insomnia
- Difficulty with concentration or memory
Understanding the Challenges of Living with PCS
PCS is a common complication of concussions. Research shows that the prevalence of persistent concussion systems is between 10% and 41.5%. However, life after post-concussion syndrome appears different for every individual.
You may notice that symptoms are affecting your ability to work or maintain social interactions. Or you could experience severe fatigue, cognitive difficulties, and symptoms of depression.
Even after recovering from PCS, some lingering effects may require you to make a few adjustments to navigate daily activities and support long-term health. Since each person’s journey with PCS is unique, it is important to seek adequate diagnosis and work with physicians who can develop tailored treatment plans around your needs.
Physical Limitations
Concussions can cause physical symptoms. For example, headaches are a common issue after a traumatic brain injury that should ease down as the brain’s tissues heal. However, in 30% of cases, this symptom continues to occur after six months of the injury.
Daily limitations can occur due to ongoing headaches and pain. Altered brain signal processing may also cause sensory overload, making you more sensitive to light and noise—worsening headaches and dizziness. While often attributed to brain injury, many of these symptoms actually stem from the upper cervical spine. Known as cervicogenic symptoms, they may result from muscle strain, joint dysfunction, or ligament laxity around the C0–C2 vertebrae. These neck issues can disrupt nerve signaling and blood flow, intensifying symptoms and delaying recovery if left undiagnosed.
These challenges make routine tasks such as driving, shopping, or participating in social activities exhausting and often overwhelming.
Unpredictable Symptoms
Living with PCS can feel like a rollercoaster because symptoms can change unpredictably from day to day. On some days, changes in blood flow or inflammation in your brain might trigger a bad day with intense symptoms. Other days, you might feel almost normal.
Since it’s hard to predict when symptoms might flare up, you may feel anxious and struggle to plan your daily activities. Additionally, PCS symptoms are often misdiagnosed. This can complicate the situation further, as you may not be sure about what you are dealing with and how long it will take to recover.
Balancing Work, Relationships, and Daily Challenges
Post-concussion symptoms often stem from changes in the brain caused by a concussion. This can lead to cognitive issues like inability to focus, memory problems, and mood swings. Research also found that severe chronic fatigue is a common symptom after concussion and that 73% of people continue to be affected five years after their injury.
These limitations can make it difficult to balance work, relationships, and daily challenges. Cognitive struggles can lead to decreased productivity at work or in academic settings. Relationships may suffer due to emotional challenges, and daily activities become stressful as you are required to adjust to changing symptoms.
Emotional and Psychological Toll
Emotional and psychological complications occur when the brain injury disrupts the release of chemicals in the brain—known as neurotransmitters—responsible for regulating mood and emotions. These include:
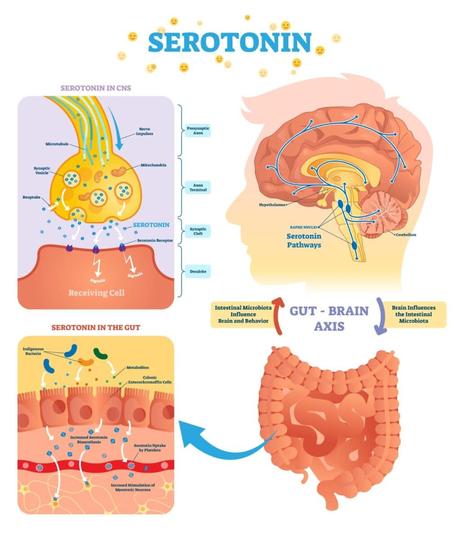
- Serotonin: This is often referred to as the “feel-good” neurotransmitter. It helps regulate mood, and low levels can lead to depression and anxiety.
- Dopamine: This chemical is involved in mechanisms like reward and pleasure. Altered levels can cause a lack of motivation.
- Norepinephrine: Norepinephrine influences attention and your body’s response to stress. Imbalances may lead to excessive anxiety and stress responses.
- GABA (gamma-aminobutyric acid): GABA acts as a calming agent in the brain. When levels fall below normal, you may feel anxious, irritable, and restless.
- Acetylcholine: This neurotransmitter plays a role in memory and learning. When disrupted, it may result in cognitive difficulties and memory impairment.
In PCS, these neurotransmitter changes can lead to emotional problems, impacting relationships, self-esteem, and overall well-being.
Financial Struggles
Post-concussion syndrome can also lead to financial challenges. Medical expenses for treatments and consultations can accumulate. This can be made worse by an inaccurate diagnosis, which can cause you to buy ineffective medications.
Other financial strains come from the fact that physical, cognitive, and emotional challenges lead to reduced work capacity or job loss. In a study published in Nature magazine, individuals with PCS visited health services 68 times on average, compared to only five times for acute concussion patients. Patients also reported missing three workdays in the previous week due to symptoms.
These financial stresses make medical care even less affordable, which kick-starts a downward spiral. Navigating disability benefits, reduced productivity, and growing medical bills can take a significant toll on your mental and physical health.
Navigating Healthcare and Finding Proper Support
Despite its high prevalence, PCS remains a challenging condition to manage. This is often because of healthcare barriers, including:
- Lack of specialized care: Finding healthcare providers who understand PCS can be difficult. Without specialized care, you might receive inadequate treatment.
- Insurance issues: Insurance often doesn’t cover all PCS treatments, especially interventions like acupuncture and physical therapy. This can make it hard for you to afford the necessary therapies.
- High misdiagnosis rates: PCS symptoms often resemble other conditions, leading to high rates of misdiagnosis. This can cause delays in getting the right treatment.
To overcome these barriers, it is crucial to consult specialists who can provide tailored support and guidance, helping you navigate the challenges of PCS treatment and recovery.
Coping Strategies for Managing PCS
Living with post-concussion syndrome can bring its own set of challenges. Some struggle with emotional challenges that impact their relationships, making it hard to connect with loved ones. Others might find that physical limitations make it difficult to keep up with work and daily tasks.
Combining various methods, such as medical support, therapy, and participation in support groups, plays a pivotal role in your recovery journey. Some approaches that should be part of a comprehensive PCS management plan include:
- Acknowledge Common Challenges
The first step is to work with your physician to understand the common symptoms and challenges associated with PCS. Recognizing these challenges helps validate your experience and empowers you to deal with them directly. This is also important to develop a treatment plan that addresses different aspects of this condition.
Common problems you may face in your journey to recovery include:
- Sleep disturbances: PCS can lead to chronic pain and disrupt your brain’s sleep-wake cycle. This makes it challenging to fall and stay asleep, leading to insomnia, poor rest, and feelings of exhaustion.
- Low energy levels and fatigue: The brain requires more energy to heal damaged tissues and restore normal chemical balance. This, coupled with symptoms like headaches, can affect your energy levels.
- Chronic pain: Ongoing headaches or neck pain from PCS can interfere with your work and personal life.
- Difficulty concentrating: Disrupted neurotransmitter signals can make focusing difficult, impacting your job performance and daily tasks.
- Emotional health challenges: Imbalances in brain chemicals can cause mood swings, anxiety, or depression, straining relationships and affecting mental well-being.
- Practical Daily Strategies for Symptom Management: Besides specific therapies, daily practices and your lifestyle can play a role in supporting your recovery. Some approaches include:
- Pace activities: By spreading activities throughout the day and taking breaks, you can reduce cognitive load and better manage fatigue, giving the brain time to recover and adapt without worsening symptoms.
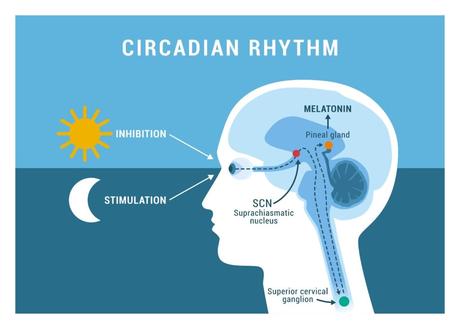
- Manage screen time: Research published in The Cureus Journal of Medical Science shows that excessive screen time can have a detrimental impact on mental health, increase the risk of anxiety and stress, and disrupt sleep patterns by altering the production of melatonin, the “sleep hormone.” Limiting screen exposure, especially before bed, can support better sleep and reduce the intensity of headaches and eye strain.
- Avoid overstimulation: Minimizing exposure to loud noises and bright lights helps prevent anxiety and allows neurotransmitter levels to stabilize. This can support brain healing and prevent symptoms from worsening.
- Prioritize rest: Taking regular breaks helps prevent overexertion. Rest allows your brain to reset its chemical balance, promote relaxation, and support the processes necessary for tissue healing.
- Physical and Mental Well-Being: Certain lifestyle modifications can support your mental and physical health. In turn, improved overall wellness can speed up healing and recovery. Possible interventions include:
- Proper nutrition: Nutrients such as omega-3 fatty acids, antioxidants, and magnesium support brain function and repair by reducing inflammation and oxidative stress.
- Light exercise: Activities like walking or gentle yoga can improve blood circulation and increase endorphin levels. The body functions can naturally boost mood and increase pain tolerance levels, helping you better cope with your symptoms.
- Mindfulness and relaxation techniques: Practices like meditation or deep breathing activate the parasympathetic nervous system, reduce stress hormones, and lower pain perception, easing both mental and physical symptoms.
- Environmental Adjustments for a More Manageable Routine: The environment plays a critical role in managing life after post-concussion syndrome. Certain adjustments can help reduce symptom triggers, minimize overstimulation, and take into account the cognitive or physical limitations you are experiencing. These include:
- Workplace modifications: Make changes to reduce sensory overload and support good posture. For example, try adjusting lighting to reduce glare and brightness on screens, or using ergonomic furniture to ease physical strain. Also, create a flexible schedule that accommodates breaks. Together, these steps can help reduce fatigue and mental stress.
- School accommodations: Use a quiet study area and noise-canceling headphones to minimize distractions. Additionally, speak to the staff to request extended deadlines and recorded lectures, which can reduce cognitive pressure and make learning more accessible when dealing with concentration problems.
- Home adjustments: Create a peaceful environment with controlled light and sound levels to alleviate sensory issues. Also consider reducing clutter, which can cause the brain to work harder to focus and cut out distractions.
- Support Systems and Resources: Accessing the right support systems is essential to optimize overall well-being and recovery. Key players include:
- Medical guidance: Regular consultations with healthcare professionals can help you access tailored treatment plans. Additionally, continuous monitoring is important to adjust therapies based on progress and symptom changes.
- Therapy and counseling: Recent research shows that nearly half of patients with PCS also experience depression symptoms. Psychological support can help address the mental health impact and develop coping strategies for anxiety, depression, and emotional regulation.
- Support groups: Connecting with others facing similar challenges can validate your feelings, teach you new coping strategies, reduce isolation, and offer the opportunity to share experiences.
- Encouragement and Patience: PCS recovery isn’t always a straight path. You are likely to enjoy progress but also experience setbacks. In this journey, patience is key. Develop a trusted treatment plan with your healthcare provider and stick to it. Work with specialists and support groups to learn about coping strategies, set realistic goals, and don’t overlook the importance of celebrating small victories along the way.
This comprehensive approach equips you to manage challenges and encourages you to stay committed, ultimately improving your quality of life.
Why Some Patients Struggle to Recover Fully
Sometimes, PCS symptoms may persist despite treatment. Causes include misdiagnosis, overlooked neck injuries, and unresolved neurological issues. When living with post-concussion syndrome, it is critical to understand and tackle the root causes of ongoing symptoms to support recovery.
Factors That May Delay Recovery
Recovery from PCS is a complex process influenced by various factors, some of which are often overlooked. Recognizing these can be crucial for managing your symptoms effectively and making progress.
- Excessive screen time: Prolonged exposure to screens can disrupt the wake-sleep cycle and aggravate PCS symptoms like headaches and eye strain. The rapid movement and bright light emitted by screens can also overstimulate the visual cortex and affect the brain’s ability to process information. These stimuli can lead to neural fatigue, impaired cognitive function, and the worsening of symptoms like dizziness and concentration difficulties.
- Driving too soon: Driving or operating machinery requires intense focus, coordination, and quick reflexes. This can lead to unnecessary stress and brain fatigue after a concussion. Additionally, the vibrations and noise associated with driving can also intensify sensory overload and stress, disrupting neural processing.
- Not to be overlooked: PCS often compromises reaction times and spatial awareness, increasing the risk of accidents.
- Listening to loud music or using headphones: Exposure to loud sounds, particularly through headphones, can cause overstimulation of the auditory pathways, overstressing the auditory cortex. This leads to worsening symptoms like headaches, dizziness, and concentration issues.
- Unapproved physical activity: Joining in on physical activities too soon can harm your recovery. High-impact exercises may misalign your spine and strain already damaged tissues, increasing injury risk and slowing down healing. Staying active is essential for overall well-being, but choose exercises your physician approves, focusing on balance and gradually building strength.
- Risk of a second head injury: Suffering a second concussion before fully recovering from the first, known as second impact syndrome, can have severe consequences, including swelling and compounded cognitive deficits. After the initial injury, the brain is more vulnerable, using energy to heal damaged tissues. An additional trauma can drastically increase recovery time and symptom severity, sometimes leading to life-threatening complications.
- Misdiagnosis and Undetected Underlying Conditions
As noted above, PCS is often misdiagnosed as its symptoms mimic the ones of other conditions, such as craniocervical instability (CCI). An inaccurate diagnosis can delay and misguide treatment, delaying recovery. Additionally, without proper identification, underlying conditions remain unchecked, increasing the risk of complications.
- Undiagnosed Cervical Injuries
Often, undiagnosed injuries to the cervical spine, or the neck, can cause persistent headaches, dizziness, and cognitive dysfunction, which are similar to PCS symptoms. These injuries lead to instability in the cervical region, causing improper neural feedback and severe symptoms. Utilizing advanced diagnostic procedures ensures these spinal issues are identified and treated.
The Centeno-Schultz Expertise in Identifying Causes of Prolonged PCS Recovery
At the Centeno-Schultz Clinic, we understand that your experience of living with post-concussion syndrome is unique. Your symptoms and journey to recovery may be influenced by factors that aren’t immediately obvious, such as CCI.
This condition occurs when the upper neck ligaments are too loose, allowing excessive movement between the skull and spine. This instability can worsen PCS symptoms like headaches and dizziness and can make recovery more difficult. Conversely, untreated PCS can increase neck instability over time, increasing the risk of complications.
In these cases, medications to manage chronic pain are not enough: they won’t address the root cause of your symptoms and can expose you to side effects. That’s why accurate diagnosis is crucial. By relying on physicians specializing in advanced diagnostics, you can uncover these hidden factors and receive a tailored treatment plan, helping you address all aspects of your condition.
Advanced Digital Motion X-ray Detection of Neck Issues in PCS Patients
At the Centeno-Schultz Clinic, we utilize advanced diagnostic techniques like DMX to better understand and treat your condition.
Unlike static X-ray images, DMX captures your body in motion. This dynamic imaging offers important insights into how your joints and ligaments function during movement. This approach helps us identify issues that aren’t visible with traditional imaging.
By observing movement, we can observe how alignment and joint stability are impacted, crucial for diagnosing conditions like CCI. DMX can yield 100% accuracy in detecting traumatic injuries with no false positives. This precision allows us to develop targeted treatment plans, ensuring that we address all the factors impacting your recovery.
Find Accurate Diagnosis at the Centeno-Schultz Clinic
Accurate diagnosis is the essential foundation for any treatment plan for PCS. However, often, basic diagnostic methods aren’t sufficient to determine what’s at the root of your symptoms.
At the Centeno-Schultz Clinic, advanced diagnostics like Digital Motion X-ray allow our physicians to precisely identify underlying issues, such as CCI. By uncovering these root causes, we can tailor therapies to your unique needs.
Relief begins with the right diagnosis. Schedule a consultation today for an evaluation!

