Your low back pain is constant. Physical therapy, stretching, acupuncture, medications, and steroids all failed to take away the pain. Your doctor referred you to a surgeon who recommended a lumbar fusion, in particular, L 4/5 Fusion.
What is it? What are the indications that you need L4/5 Fusion? Is it a Major Surgery? What is the success rate of spinal fusion? What are the complications associated with spinal fusion? Is there an alternative to fusion surgery Let’s dig in.
What is L 4/5 Fusion Surgery?
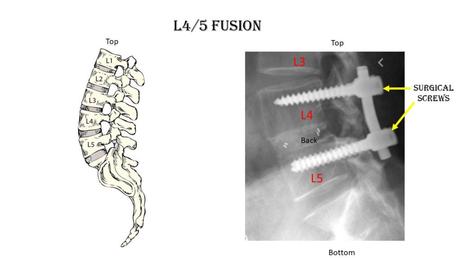
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer.
L 4/5 Fusion refers to the level of the surgery.
There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between. For example, the second-lowest disc in the low back is the L4/5 disc. The L4/5 disc is sandwiched between the L4 and L5 spinal bones. Therefore, L 4/5 Fusion surgery involves the surgical removal of the L4/5 disc and fusing the L4 and L5 spinal bones together. This is illustrated below.
What Are the Indications for L 4/5 Fusion?
Lumbar fusion is a popular surgery. Between 1998 and 2008, the yearly number of lumbar fusion surgeries performed in the United States increased from 77,682 to 210,407 (1). Lumbar fusion can be used to treat a number of painful and degenerative conditions in the low back (2). The most common indications for L4/5 fusion include:
- Low Back Disc Degeneration
- Slipped Disc (Spondylolisthesis)
- Spinal Bone Fracture
- Recurrent Disc Herniation
- Pain Radiating Down Leg (Sciatica )
- Curvature (Scoliosis)
- Narrowing of the Canal (Stenosis)
- Failed Spine Surgery with Instability
Is Spinal Fusion a Major Surgery?
Absolutely! The surgery involves cutting through important muscles, ligaments, and tendons to access the targeted disc. The disc is then removed and the area is packed with bone and often times a spacer. To stabilize the spine, screws are placed into the spinal bones above and then below the disc that is removed. The screws are stabilized by additional hardware including plates and rods.
What Is the Success Rate of Spinal Fusion Surgery?
Lumbar fusion surgery has significant risks and complications. There is an increasing amount of evidence against spinal fusion. Let’s review.
2018 study analyzed the data from 33 randomized controlled trials and other studies comparing spinal fusion to nonoperative solutions for low back and degenerative conditions (3). Of the 33 reviews, there was only one high quality, unbiased randomized control study that found “clinically meaningful benefits of fusion”. All the other studies found elective fusion to be no more effective than conservative therapy.
A 2015 study randomized participants into two groups: a surgical fusion group and a nonsurgical, conservative therapy group (4). Back pain, quality of life, and disability were found to be no better with spinal fusion than without.
A different 2015 study demonstrated that spinal fusion for patients with Stenosis improved pain and function no better than physical therapy. (5)
A 2018 study that followed patients after lumbar fusion noted that 91% were still on narcotics (6). Regrettably, 45% were taking higher doses after surgery than before.
What are the Complications Associated with Spinal Fusion Surgery?
The number of complications from spinal fusion surgery is extensive. They can be divided into two principal groups: Immediate and Long-term complications.
Immediate complications are those that occur during the time of surgery or immediately thereafter. They include bleeding, infection, escalation in pain, and nerve damage.
Long-term Complications
Non-union
Non-union occurs when the spinal bones that are bolted together fail to fuse or grow together. Rates vary depending upon the specific type of lumbar spinal fusion procedure. For procedures that require more bone, like a posterior fusion, the non-union rates are as high as 26-36% (7,8).
Hardware Breaking
Lumbar fusion involves screws, bolts, and plates that stabilize the spinal bones. There are significant forces placed on the low back and the hardware. Regrettably, as a result of these forces, the hardware can break creating spinal instability and pain. The incidence of hardware failure in one study was an alarming 36% (9). Treatment of hardware failure often requires additional surgery to remove the broken hardware and replace it.
Hardware Becoming Loose
Screws are used in lumbar fusion to stabilize the spine. The same forces that can cause the hardware to break can also cause the screws to become loose. This, in turn, can create spinal instability and pain. Collectively about 1 in 10 patients who have a low back fusion will need a second surgery to fix non-union or hardware failure (10).
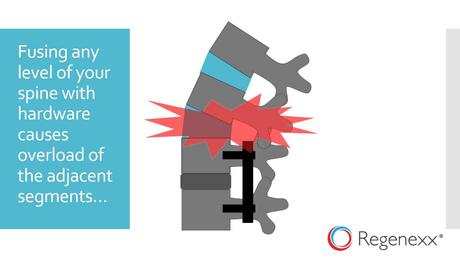
Adjacent Segment Disease
The disc is an important shock absorber. Fusion surgery removes this important shock absorber which places additional stress and forces on the discs and facet joints above and below the level of the fusion. This additional force in turn can lead to injury of these facet joints and discs leading to degeneration, arthritis, and pain. This is a real problem, with an incidence of 9% (11). This can lead to additional surgeries including fusions. To learn more about this tragic complication please click on the video below.
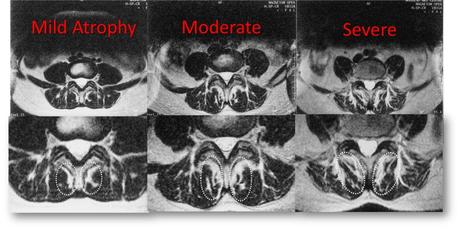
Spinal Muscle Injury
The spinal muscles provide critical stability and support for the spine. The multifidus is a spinal muscle located deep in the low back. The multifidus is a major stabilizer of the spine. Unfortunately, lumbar fusion significantly compromises the health and integrity of this muscle (10). The mulifiidus muscle can actually shrink in size which is called atrophy. This is in turn can lead to spine instability, degeneration, arthritis, and pain. While this is easy to see on MRI it is rarely commented on by the radiologist. Below are MRI images of the lumbar spine in cross section. Progressive atrophy is shown from left to right.
Is There an Alternative to L 4/5 Fusion Surgery?
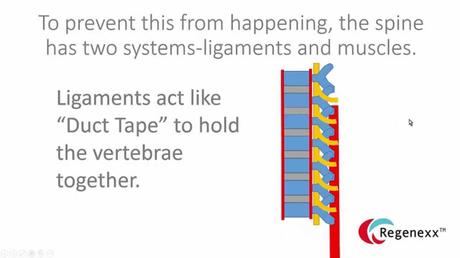
Absolutely. At the Centeno-Schultz Clinic, we believe in a comprehensive approach to the treatment of low back pain. We view and approach the spine as a Functional Spinal Unit. This functional unit includes discs, facet joints, ligaments, fascia, and muscles. These structures work with one another in a highly specialized and dependent manner. Therefore for the very best results, the spine and all its parts need to be evaluated and treated together. This novel, comprehensive approach can help you avoid lumbar fusion and its complications. Treatment options include PRP and your own bone marrow-derived stem cells. PRP is rich in growth factors which can increase blood flow and healing. To better understand how to avoid lumbar fusions by using precisely guided PRP and stem cell injections please click on the video below.
In Conclusion
Spinal fusion is a major surgery where one or more spinal bones are fused together using screws, bolts, and plates. L 4/5 fusion involves the removal of the L4/5 disc and fusing the L4 and L5 vertebral bones. The indications for L 4/5 fusion are numerous and include low back disc degeneration, slipped disc, spinal bone fracture, recurrent disc herniation, scoliosis, and stenosis. There is an increasing number of high quality, unbiased studies that demonstrate that lumbar fusion is no better than conservative care. There are numerous complications associated with L 4/5 fusion which include non-union, hardware breakage, adjacent segment disease, and multifidus atrophy. At the Centeno-Schultz Clinic, a comprehensive approach is utilized in the evaluation and treatment of low back pain. The spine is viewed as a functional spinal unit as opposed to a collection of separate structures. Treatment options include PRP and a patient’s own stem cells. Our treatment outcomes are here.
If you or a loved one has ongoing low back pain please schedule a telemedicine consult. Learn from board-certified, fellowship-trained physicians your nonsurgical treatment options. L4/5 fusion is a major surgery associated with significant complications that forever changes the stability and architecture of your spine. Make a better decision!
References
1.Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67–76.
2.Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine. 2019;31(1):1-14. doi:10.3171/2019.4.SPINE18915
3.Harris IA, Traeger A, Stanford R, Maher CG, Buchbinder R. Lumbar spine fusion: what is the evidence?. Intern Med J. 2018;48(12):1430-1434. doi:10.1111/imj.14120
4.Hedlund R, Johansson C, Hägg O, Fritzell P, Tullberg T; Swedish Lumbar Spine Study Group. The long-term outcome of lumbar fusion in the Swedish lumbar spine study. Spine J. 2016;16(5):579-587. doi:10.1016/j.spinee.2015.08.065
5. Delitto A, Piva SR, Moore CG, Welch WC. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis. Ann Intern Med. 2015;163(5):397-398. doi:10.7326/L15-5129-4
6. Deyo RA, Hallvik SE, Hildebran C, et al. Use of prescription opioids before and after an operation for chronic pain (lumbar fusion surgery). Pain. 2018;159(6):1147-1154. doi:10.1097/j.pain.0000000000001202
7.Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(8):1107–1112. doi: 10.1007/s00586-008-0695-9.
8.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991 Jul; 73(6):802-8. https://www.ncbi.nlm.nih.gov/pubmed/2071615/.
9.Harris IA, Traeger A, Stanford R, Maher CG, Buchbinder R. Lumbar spine fusion: what is the evidence. Intern Med J. 2018;48(12):1430-4.
10. Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976). 2004 Nov 15;29(22):2516-20.
11. Ghiasi MS, Arjmand N, Shirazi-Adl A, et al. Cross-sectional area of human trunk paraspinal muscles before and after posterior lumbar surgery using magnetic resonance imaging. Eur Spine J. 2016;25(3):774-782. doi:10.1007/s00586-015-4014-y

