Post-concussion syndrome (PCS) is a complex disorder that may develop after experiencing a concussion. It occurs when symptoms persist beyond the typical recovery time frame of three months, sometimes indicating deeper issues with the neck or nerves.
PCS is characterized by symptoms like persistent headaches, dizziness, and cognitive disturbances. These symptoms can significantly disrupt everyday life, affecting work, social interactions, and family dynamics.
An accurate diagnosis is essential to address underlying issues and support long-term musculoskeletal health. Advanced diagnostic tools, such as digital motion X-ray (DMX)or upright MRI with flexion-extension views, along with interventional orthobiologic options offered by physicians at the Centeno-Schultz Clinic, provide non-surgical alternatives designed to support the body’s natural healing processes. These approaches may treat the true cause of your ongoing symptoms. Read on to learn more.
Understanding the Post-Concussion Syndrome Recovery Timeline
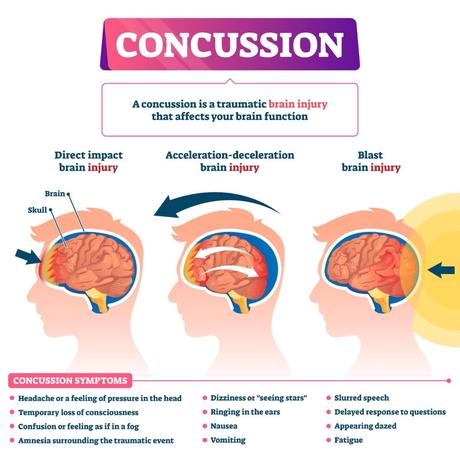
A concussion can result from a jolt or blow to the head, triggering a cascade of reactions within the brain. These include:
- Axonal shearing: Damage to the brain’s tissues, or axons, which disrupts neural communication.
- Inflammation: The inflammatory response to injury causes swelling and increased sensitivity within brain tissue, leading to bruising, pain, and headaches.
- Neurotransmitter imbalance: Following an injury, the brain can release abnormal levels of chemicals like neurotransmitters. These altered chemical signals overstimulate neurons and interfere with neural communication and brain function.
However, another common issue is upper neck trauma. More on that below.
According to a 2023 study, around 90% of concussion symptoms are temporary and resolve within 10-14 days as the brain stabilizes and repairs itself. However, in some cases, these symptoms persist, leading to PCS. PCS arises when the brain’s recovery process takes longer than the expected timeline. It can stem from secondary upper neck injuries that often go undiagnosed.
Recovery from PCS can be unpredictable: symptoms may last for months or even years. This syndrome requires a comprehensive, patient-focused approach to manage persistent symptoms, address underlying issues, and support recovery.
Here’s a general timeline of PCS:
Acute Phase (0–7 days)
In the acute phase, symptoms are similar to those experienced immediately after the concussion. Physical symptoms include headaches, dizziness, and fatigue. Other signs include:
- Sensory disturbances such as light or sound sensitivity.
- Cognitive difficulties, like memory and concentration issues.
- Emotional changes, including irritability or sadness.
Rest is crucial during this time. Avoid activities that can worsen symptoms. A gradual return to daily routines under professional guidance is recommended.
Subacute Phase (7–28 days)
In the subacute phase, some symptoms may begin to improve or stabilize. As the brain begins to heal, you may regain some physical and cognitive functions. During this phase, physicians may recommend short periods of activity followed by rest.
Persistent Phase (4+ weeks)
Up to 43% of concussion patients experience PCS, with symptoms like fatigue, headache, depression, and difficulty concentrating persisting for three months or longer. This happens when the brain doesn’t heal fully or when tissue damage lasts longer than expected. Common underlying problems include disruptions to neural pathways, nerve damage, and upper neck problems. In our experience, this last one, undiagnosed upper neck injuries, are a very common cause of delayed recovery.
Here are some specifics about this phase:
- Symptoms extend beyond the typical recovery period of three to four weeks.
- Underlying conditions, like migraines or anxiety, can aggravate or prolong symptoms.
- Chronic inflammation causes swelling and increased sensitivity to pain.
- Long-term symptoms often interfere with cognitive and physical activities, impacting work and social interactions.
- Collaboration among patients, families, and healthcare providers is important to understand and manage symptoms better.
- Getting a thorough, hands-on upper neck exam and appropriate imaging is key. Note that a routine MRI will often miss the signs of an upper neck injury.
Associated Symptoms Present During Post-Concussion Recovery
PCS is associated with a range of symptoms that can affect physical, emotional, and cognitive health. The presence and intensity of these signs vary, impacting daily activities and overall well-being.
Physical Symptoms
Physical symptoms during post-concussion stem from damage or strain of the tissue of the brain or neck. These include:
- Headache: Persistent or throbbing headaches are common. This happens when pain-sensitive areas in the brain and scalp become overly active and inflamed. Research shows that up to 90% of individuals experience headaches soon after a traumatic brain injury (TBI). Approximately 30% still have headaches after six months, and around 58% continue for a year or longer.
Having said that, a common cause of headaches in post-concussive patients is upper neck injury. The upper neck facet joints can refer pain into the head and are often injured in head trauma. In addition, the occipital nerves are another common cause.
- Neck pain: Stiffness or discomfort often arise from whiplash or impact, which can strain muscles and damage joints. Additionally, neck injuries can damage or compress nerves, leading to symptoms like numbness, tingling, and muscle weakness. These symptoms tend to radiate from the neck to the head, shoulder, arms, and hands.
- Blurred vision: Problems in the brain’s visual processing pathways can cause light sensitivity and eye strain after reading and screen use.
- Dizziness: Changes in the balance system affect how the body perceives movement (proprioception). This can lead to symptoms like dizziness and vertigo.
- Fatigue: After a concussion, the brain works harder to support healing and maintain function. This uses up energy, leading to exhaustion and constant tiredness despite rest.
- Sleep disturbance: Patterns like insomnia or excessive sleep occur when the brain’s sleep control centers get disrupted.
Emotional Symptoms
PCS can lead to emotional issues because injuries can disrupt neurotransmitter functions and alter brain chemistry, affecting mood regulation areas. These changes may cause anxiety, depression, and irritability. Additionally, prolonged physical symptoms and stress from recovery can aggravate emotional distress. Finally, chronic pain from the upper neck can also lead to poor sleep and emotional exhaustion.
Emotional symptoms include:
- Irritability
- Anxiety
- Depression
- Emotional instability
- Stress
Appropriate emotional support, counseling, and stress management techniques—like mindfulness and relaxation exercises—can assist in managing these symptoms.
Cognitive Symptoms
Cognitive symptoms in PCS occur because brain connections get disrupted. Damage to specific brain cells affects the areas that control memory, focus, and quick thinking. Also, low energy in brain cells makes it hard to process information, leading to confusion and difficulty concentrating.In addition, upper neck problems also cause problems like brain fog.
Common cognitive symptoms include:
- Memory issues
- Poor concentration
- Slower processing speed
- Impaired decision making
- Confusion
- Brain Fog
Cognitive rehabilitation therapies should be part of a broader recovery strategy, including memory exercises, structured routines, and gradual re-engagement with complex tasks.In addition, this may also involve getting the upper neck treated.
Common Factors That May Affect Recovery Time
Recovery periods can vary depending on several factors. Studies suggest that risk factors for persistent PCS include complicated or multiple traumatic brain injuries, being female, age, and a history of psychiatric disorders and chronic pain syndromes. In addition, undiagnosed upper neck injurioes are a common caus. Understanding these factors helps in anticipating recovery trajectories and tailoring individualized care plans.
Age and Overall Health
Older adults may experience prolonged symptoms due to slower cellular repair mechanisms. Slower regeneration rates mean that the healing of damaged tissues takes longer.
Additionally, overall health impacts recovery, including physical fitness and immune function. Good health enhances recovery by boosting the immune system, reducing inflammation, and supporting brain function with proper nutrition and rest.
Previous Concussions
Having a history of previous concussions can complicate recovery. Repeated injuries may lead to cumulative effects, increasing the likelihood of persistent symptoms.
Additionally, the brain’s resilience can weaken after each incident, extending recovery time and affecting neural plasticity, which is essential for recovery.
Severity of the Concussion
More intense traumas typically result in more severe damage to brain and neck issues, extending recovery. Additionally, severe concussions cause greater disruption in neuronal signaling, which can make symptoms particularly impactful. In turn, a significant decline in physical and cognitive abilities can make recovery more complicated.
Undiagnosed Upper Neck Injuries
The head is attached to yoour upper neck with ligaments and joints. Therefore, if your head sustains trauma, manytimes these structutres are injured as well. Despite neck injuries in PCS patients bieng common, few patients get these issues diagnosed. Why?
- Many PCS patients see providsers who are not expert in diagnosing these injuries.
- Routine neck MRIs don;lt show the upper neck in great detail.
- Many PCS patients have craniocervical instability whioch requires specialized movement-based imaging.
Lifestyle Factors
Lifestyle choices, such as physical activity level and stress management, influence recovery. Regular exercise may promote brain health and speed up recovery by increasing cerebral blood flow. On the other hand, high-stress levels can aggravate symptoms by triggering the release of high cortisol levels, impacting brain recovery and cognitive function.
Chronic Conditions
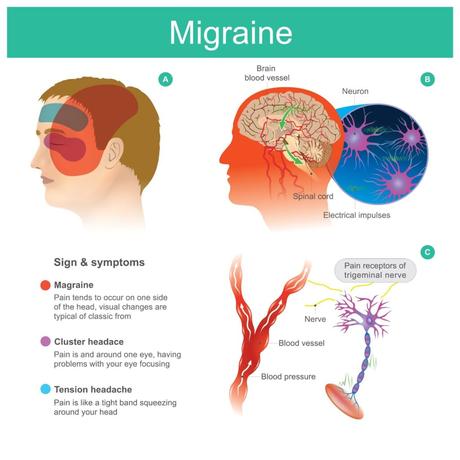
Existing chronic conditions, such as migraines or depression, can prolong PCS recovery. These conditions can worsen concussion symptoms by affecting neurochemical balance and heightening sensitivity to stimuli. Managing these conditions is critical to prevent them from interfering with the healing process.
Sleep Patterns and Fatigue
Poor sleep quality and fatigue significantly impact recovery. Sleep is an essential body function necessary for several processes, including memory management and tissue regeneration. Studies confirm that sleep is also essential for cognitive recovery after injuries.
Disrupted sleep, which is often a consequence of CPS, headaches, and brain injuries, can impair memory consolidation and neuroplasticity, essential for healing. Adequate rest and sleep hygiene should be considered vital components of a successful recovery strategy.
Signs That Your Recovery Is Taking Longer Than Usual
Symptoms that persist after the expected healing timelines, like headaches and cognitive problems, may suggest underlying conditions, which may require professional evaluation. Some common symptoms after a concussion that may warrant medical attention include:
Ongoing Dizziness and Balance Problems
Dizziness and balance issues that persist over time may point to vestibular or upper neck dysfunction, a disorder affecting the inner ear, brain, or cervical spine. Vestibular and upper neck dysfunction leads to balance issues and dizziness, which affect daily activities and increase the risk of falls and further injuries.
Persistent Headaches
Ongoing headaches post-concussion might suggest underlying tension or migraines that affect the neural processes in the brain. Research indicates that concussion patients are at greater risk of developing migraines compared to those who have never experienced a brain injury.
It’s critical to realize that a major source of ongoing headaches in PCS patients is the upper neck. For example, the C0-C3 upper neck joints, when injured, refer pain to the head. In addition, the occipital nerves also cause headaches and muscle spasm or tightness at the base of the skull often cause these nerves to be irritated. Getting these conditions diagnosed requires specialized care and expertise not usually found in the providers many PCS patients use to treat and manage concussion.
Ongoing and severe headaches disrupt daily life, hinder concentration and work performance, and prolong recovery. A thorough evaluation can determine the headache type, guiding effective treatment like medication and lifestyle changes for better management.
Cognitive Difficulties
Lasting cognitive issues after a concussion indicate ongoing neural disruption, which changes in the brain chemistry or structure can cause. For example, prolonged inflammation in the brain can lead to memory and focus issues. Early action is important to restore mental function and facilitate the return to all daily activities.
Insomnia
As noted above, sleep plays a critical role in supporting the repair of damaged tissues and in restoring cognitive functions. Additionally, poor sleep increases fatigue and reduces cognitive abilities, making recovery even more complicated.
If you are experiencing insomnia and sleep disruptions long after a concussion, it is important to evaluate the causes and adopt strategies like sleep hygiene and therapy to support your recovery.
Sensitivity to Light and Noise for Extended Periods
Long-term sensitivity to light and noise suggests issues with the brain’s processing pathways, which are the networks that manage sensory information like light. These symptoms can severely disrupt daily life and social activities and aggravate other issues like headaches, migraines, and dizziness.
Impact of Prolonged Post-Concussion Syndrome on Daily Life
Experiencing prolonged PCS brings several challenges that hinder the ability to carry out everyday activities. These difficulties can transform routine tasks into major hurdles, affecting all facets of life. Common complications include:
- Impact on physical activities: PCS causes fatigue, dizziness, and balance problems, making activities like walking tiring and altering daily routines. These symptoms can also interfere with participation in sports or activities you once enjoyed. In turn, these barriers can limit daily movements and activity levels, affecting overall health.
- Challenges at work or school: Cognitive symptoms like memory and focus issues can slow down functions like cognitive processing and decision-making at work or school.
- Effects on social life: Sensitivity to sound and light, coupled with headaches and mobility limitations, makes social events overwhelming, leading to withdrawal from activities. This can compromise friendships or romantic relationships and even cause breakdowns within a person’s support network.
- Impact on family and relationships: Emotional symptoms, like irritability, cause family misunderstandings. Additionally, relationships can be thrown off balance when there is an increased need for help in daily tasks and around-the-clock care. Additionally, if you cannot join family activities, you may feel detached and lonely.
When Recovery Issues May Indicate Upper Neck Injuries
Persistent symptoms of PCS often overlap with similar symptoms caused by underlying and often undiagnosed upper neck injuries, such as craniocervical instability (CCI) or craniocervical syndrome. These injuries can stem from the same traumatic event that caused the concussion. However, they are commonly undiagnosed during initial assessments without adequate diagnostic tools, leading to persistent symptoms.
CCI can damage the upper neck joints, impact head and neck alignment, compromise nerve pathways and blood flow, which aggravate symptoms like headaches, dizziness, and cognitive issues commonly associated with PCS. CCS or craniocervical syndrome means that the upper neck structures that cause the same symptoms as PCS were injured, but without the instability of CCI.
It is important to note that symptoms that overlap between PCS and upper neck injuries can complicate recovery and delay treatment. For example, neck pain, balance issues, and visual disturbances are hallmark symptoms in both conditions, making it challenging to identify the exact cause without specialized assessment. This highlights the importance of seeking expert diagnosis to uncover any hidden neck injuries contributing to PCS symptoms.
The Risk of Misdiagnosis: How Neck Injuries Can Mask PCS
Misdiagnosed neck injuries can significantly slow down the recovery from PCS. These injuries, if overlooked, can lead to ongoing symptoms and make treatment strategies targeting just the symptoms—and not the underlying cause—inefficient.
As neck injuries often share symptoms with PCS, diagnosing errors can occur, delaying appropriate intervention and recovery. Consequences of missing a neck injury diagnosis include:
- Continued Symptoms: Upper neck injuries can cause headache, imbalance/dizziness/vertigo, brain fog and other symptoms like autonomic dysfunction (tachycardia, POTS, etc).
- Chronic pain: Untreated neck injuries may lead to persistent pain, headaches, and muscle tension.
- Delayed recovery: Without addressing the root cause of CPS, symptoms can last longer than expected, prolonging recovery time.
- Ineffective treatment: Treatments focused solely on PCS usually won’t alleviate symptoms caused by an undiagnosed upper neck injury.
- Increased psychological stress: Ongoing symptoms without effective relief can lead to stress, anxiety, and depression. Declining mental health can affect physical well-being, starting a vicious cycle that delays recovery.
- Reduced quality of life: Unresolved injuries impact daily activities and social interactions, compounding physical and emotional distress.
Movement-based Imaging: Your Best Option for Proper Evaluation
Consulting healthcare providers for a thorough evaluation is crucial when managing potential upper neck injuries. Advanced imaging techniques, such as the Digital Motion X-ray (DMX) technology and upright MRI with flexion-extension views, are now able to capture neck movements in real-time. Unlike static imaging tests, such as X-ray and supine MRI, DMX and upright MRI provide dynamic aspects that highlight ligament issues, particularly the alar, transverse, and accessory ligaments, which play key roles in controlling neck stability.
This approach plays a crucial role in identifying CCI. Recent research, published by Freeman and Katz, suggests that the DMX method offers an excellent level of precision and accuracy in diagnosing traumatic upper neck injuries, preventing false positives.
However, accurate diagnosis requires the expertise of physicians who specialize in upper neck evaluation. This skill set is rare. For example, seeing the average neurologist, physical medicine, or pain management physician is likely to result in undiagnosed upper neck issues.
At the Centeno-Schultz Clinic, we are experts in diagnosing injuries to the upper neck like CCI or CCS. Our specialists utilize advanced diagnostics and interventional orthobiologics to develop personalized, non-surgical strategies aimed at supporting the body’s natural healing processes.The goal is not only to diagnose upper neck injuries that may be prolonging your PCS recovery, but also to effectively treat them with precise injections that can help your damaged upper neck tissues heal.
Get the Right Diagnosis at the Centeno-Schultz Clinic for Relief
At the Centeno-Schultz Clinic, expert diagnosis is the cornerstone of effective treatment for neck injuries and PCS symptoms. With a deep understanding of the symptoms and complications involved in conditions like cranio-cervical instability or craniocervical syndrome, the clinic offers cutting-edge diagnostic technologies and personalized care plans.
Contact the Centeno-Schultz Clinic today for an accurate diagnosis and discover if the Regenexx approach is right for your specific case.
Feeling stuck in recovery? Concussions may signal neck injuries. Contact the Centeno-Schultz Clinic for an evaluation today.

