The purpose of this post is to describe the similarities and differences between the symptoms and diagnostics that might be used to distinguish between COVID-19 and pericarditis. I'm interested in this because, as I've described in some detail in a prior post, I've experienced acute pericarditis and still suffer from its effects.
In addition, fatalities associated with COVID-19 are overwhelmingly associated with the elderly and people with existing chronic or temporary medical conditions, such as heart disease, lung disease, asthma, the flu, or other preexisting conditions. Of course, COVID-19 will also target people who may have compromised immune systems, including those compromised by medications they may be taking to treat a preexisting condition, such as patients suffering an acute attack of pericarditis being treated with prednisone, a corticosteroids which, like others, suppresses the immune system.
COVID-19
In 2019, a new coronavirus was identified as the cause of a disease outbreak that originated in China.
The virus is now known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease it causes is called coronavirus disease 2019 (COVID-19).
The signs and symptoms of COVID-19 compiled by WebMD based on information gathered from researchers in China, included:
- Fever 83%-99%
- Cough 59%-82%
- Fatigue 44%-70%
- Lack of appetite 40%-84%
- Shortness of breath 31%-40%
- Mucus/phlegm 28%-33%
- Body aches 11%-35%
Other symptoms may include:
- Sore throat
- Headache
- Chills
- Stuffy nose
- Nausea or vomiting
- Diarrhea
PERICARDITIS
The Mayo Clinic describes pericarditis is swelling and irritation of the pericardium, the thin sac-like membrane surrounding the heart. Pericarditis often causes chest pain and sometimes other symptoms. The sharp chest pain associated with pericarditis occurs when the irritated layers of the pericardium rub against each other.
Depending on the type pf pericarditis, its signs and symptoms may include some or all of the following:
- Sharp, piercing chest pain over the center or left side of the chest, which is generally more intense when breathing in
- Shortness of breath, especially when reclining
- Heart palpitations
- Low-grade fever
- An overall sense of weakness, fatigue or feeling unwell
- Cough
- Abdominal or leg/feet swelling
COVID-19 or PERICARDITIS?
I am day 11 into COVID-19. I'm in the emergency room with severe chest pain and breathing problems. ER nurse said my heart and lungs may be inflamed. My ECG is "abnormal." My pulse is strong. I can’t get to my regular doctor because of the lock-down here. In the last 2 days since my visit to ER I have felt dizzy and nauseous. I have pain in middle of my chest and a panicky fluttery feeling. Now I have a really sore throat. Is this now pericarditis?
Answering the question of this patient on the basis of this information isn't straight-forward. As the symptoms described in the previous sections show, COVID-19 and acute pericarditis symptoms mirror each other closely. This is further illustrated in Table 1, below.
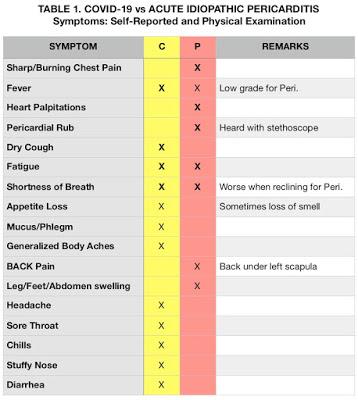 Research indicates that the most common cause of idiopathic pericarditis "in developed countries" is a virus of unknown specificity, thus the diagnosis "non-specific idiopathic pericarditis." Deriving from the severe acute respiratory syndrome coronavirus 2, COVID-19 may well trigger pericarditis, or in a patient with the pre-existing condition, a pericarditis flare up. On the other hand, patients with pre-existing cardiac conditions, like pericarditis, may be more susceptible to COVID-19 because of a disease-induced depressed immune systems, or because a treatment protocol for their pericarditis depresses their immune system, e.g., prednisone (see Figure 1).
Research indicates that the most common cause of idiopathic pericarditis "in developed countries" is a virus of unknown specificity, thus the diagnosis "non-specific idiopathic pericarditis." Deriving from the severe acute respiratory syndrome coronavirus 2, COVID-19 may well trigger pericarditis, or in a patient with the pre-existing condition, a pericarditis flare up. On the other hand, patients with pre-existing cardiac conditions, like pericarditis, may be more susceptible to COVID-19 because of a disease-induced depressed immune systems, or because a treatment protocol for their pericarditis depresses their immune system, e.g., prednisone (see Figure 1).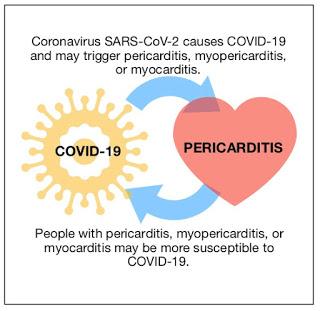
Fig. 1. Complementary relationship between COVID-19 and Pericarditis
One of the key ways humans encode and then retrieve information is by labeling and compartmentalizing it, e.g., this disease manifesting these symptoms is COVID-19. This disease manifesting these symptoms is the flu. This disease manifesting these symptoms is pericarditis.
The lay person gets the sniffles concludes they have a cold, the sniffles evolves to a cough, fever, and achy body and they lament having contracted the flu. But in the midst of a SARS-CoV-2 pandemic, they might fear they've come down with COVID-19.
In diagnosing any given patient with the objective of learning and then treating the source of their misery it's imperative that physicians understand (and most do) that the patient is a living history of all that ails them. A patient that presents with flu-like symptoms, is experiencing shortness of breath, and has sharp chest pain, must give a full health history, be examined, and be given a complete laboratory workup to sort out the source of their misery, realizing that it may be generated by a combination of linked factors, i.e., COVID-19 and pericarditis. The course of treatment depends on doing this. Otherwise it might do more harm than good.

