Your low back pain was excruciating!. Everything made the pain worse. You agree to have spine surgery and regrettably, your pain is still there. What is Failed Back Surgery Syndrome? What are the symptoms of failed back surgery? What is the treatment for Failed Back Surgery Syndrome? Are there other complications associated with spine surgery? Are there regenerative options to treat Failed Back Surgery Syndrome? Let’s dig in.
What Is Failed Back Surgery Syndrome?
Failed Back Surgery Syndrome also called failed back is a clinical condition in which patients who have undergone low back surgery continue to have pain and dysfunction. Said another way the surgery that was intended to reduce pain and increase function FAILED. That’s right, the surgery failed. You had the surgery, struggled with the pain postoperatively, diligently participated in physical therapy and yet the pain and limitation are still there. Unfortunately, this occurs frequently. Estimates range from 20-40% of patients who undergo low back surgery will develop Failed Back Surgery Syndrome (1).
Is low back surgery the answer? Consider these facts
5-36% of patients who have lumbar disc surgery for disc herniation have a recurrence of their low back and leg pain within 2 years (2)
29.2% of patients who have lumbar stenosis and undergo have surgical decompression (laminectomy) have similar or increased pain at 12 months (3).
What Are the Symptoms of Failed Back Surgery Syndrome
Pain is the most common symptom of Failed Back Surgery Syndrome. If may be present immediately after surgery or gradually return over the following days. The severity of the pain may be the same or worse after surgery. It may be confined to the low back or can radiate into the buttock, posterior thigh, and down the leg. Other symptoms that may occur include numbness, weakness, and tingling.
What Are the Causes of Failed Back Surgery Syndrome?
Failed Back Surgery Syndrome can occur for a number of reasons which include preoperative, postoperative, and diagnostic factors.
Preoperative Factor
Obesity, smoking, workman’s compensation, ongoing litigation, and psychiatric disorders can lead to Failed Back Surgery Syndrome.
Postoperative Factor
Spine surgery involves removing important structural parts of the spine. For example, a discectomy involves the removal of a portion or the entire intervertebral disc. Laminectomy is the removal of a bone of the backside of the spine that forms and protects the spinal canal that is called the lamina. Supporting ligaments, tendons, and muscles are often damaged during these surgeries. The end result is that the spine no longer functions the same. Said another way as a result of the spine surgery there is a change in the biomechanics of the spine. A classic example is a spinal fusion. The ” diseased or injured” disc is removed and the spinal bones are fused together with screws and plates. Remember that the disc acts like a shock absorber that absorbs and transfers the forces of daily living. After removing a given disc the forces of daily living are redirected above and below the fusion. This places additional wear and tear on the discs and facet joints above and below the fusion. Over time degeneration and injury occurs along with pain.
Diagnostic Factor
The successful outcome of low back surgery is dependent on the accurate diagnosis of the patient’s etiology of pain. Surgeons are not objective as their training and philosophy are biased toward surgery. Their recommendations and treatments are not in your best interest. Consulting with a surgeon about the need for low back surgery is like asking a barber if you need a haircut.
What Is the Treatment for Failed Back Surgery Syndrome?
Being proactive is your best option. Learn about your back pain and work closely with your physician to identify all the potential sources of pain. Exhaust all conservative therapies. Key points to remember.
Avoid Low Back Surgery. There are many different types of low back surgeries. Fusion is a very popular one where the disc is surgically removed and the two spinal bones are fused together. Between 1998 and 2008 the number of fusion surgeries in the United States increased by 170.9% from 77,682 to 210,407 (4). This is big business with a significant income stream for the surgeon, the surgical center, and support staff. Is it effective? Let’s look at the literature.
- 2018 study analyzed the data from 33 randomized controlled trials and other studies comparing spinal fusion to nonoperative solutions for low back and degenerative conditions (5). Of the 33 reviews, there was only one high quality, unbiased randomized control study that found “clinically meaningful benefits of fusion”. All the other studies found elective fusion to be no more effective than conservative therapy.
- A 2015 study randomized participants into two groups: a surgical fusion group and a nonsurgical, conservative therapy group (6). Back pain, quality of life, and disability were found to be no better with spinal fusion than without.
- A different 2015 study demonstrated that spinal fusion for patients with Stenosis improved pain and function no better than physical therapy (7).
- A 2018 study that followed patients after lumbar fusion noted that 91% were still on narcotics (8). Regrettably, 45% were taking higher doses after surgery than before.
Avoid Repeat Back Surgery. Often times the surgeon will recommend a ” revision” or a second surgery to address the FAILED SURGERY and the patient’s pain. RUN! There is a good chance that the second surgery will also fail. A recent study demonstrated that no more than 30%, 15%, and 5% of the patients experience a successful outcome after the second, third, and fourth surgeries (9)
Identify the Source or Sources of Low Back Pain. Do not rely exclusively on the MRI. Have your doctor actually review in detail the MRI study and not the report. A thorough examination is essential. At the Centeno-Schultz Clinic, a comprehensive approach is utilized. We view and approach the spine as a Functional Spinal Unit. This functional unit includes discs, facet joints, ligaments, fascia, and muscles. These structures work with one another in a highly specialized and dependent manner. Therefore for the very best results, the spine and all its parts need to be evaluated and treated together. This novel, comprehensive approach can help you avoid lumbar fusion and its complications. Treatment options include PRP and your own bone marrow-derived stem cells. PRP is rich in growth factors which can increase blood flow and healing. To better understand how to avoid lumbar surgery by using precisely guided PRP and stem cell injections please click on the video below.
Are there Other complications Associated with Spine Surgery?
Yes. In addition to the failure of the proposed low back surgery to improve pain and quality of life, there are a number of other long-term complications associated with spinal surgery. Three very common complications are:
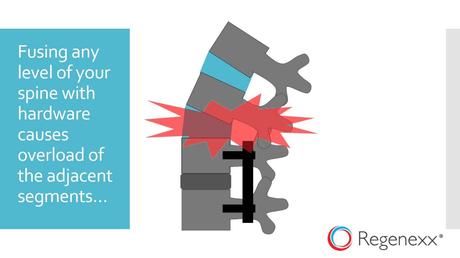
Adjacent Segment Disease
The disc is an important shock absorber. Fusion surgery removes this important shock absorber which places additional stress and forces on the discs and facet joints above and below the level of the fusion. This additional force in turn can lead to injury of these facet joints and discs leading to degeneration, arthritis, and pain. This is a real problem, with an incidence of 9% (10). This can lead to additional surgeries including fusions. To learn more about this tragic complication please click on the video below.
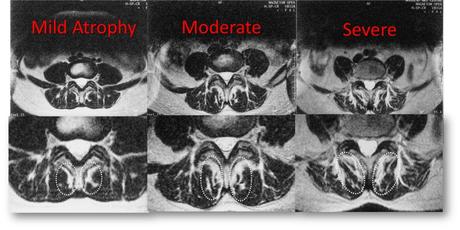
Spinal Muscle Injury
The spinal muscles provide critical stability and support for the spine. The multifidus is a spinal muscle located deep in the low back. It is a major stabilizer of the spine. Unfortunately, lumbar fusion significantly compromises the health and integrity of this muscle (11). The multifidus muscle can actually shrink in size which is called atrophy. This is in turn can lead to spine instability, degeneration, arthritis, and pain. While this is easy to see on MRI it is rarely commented on by the radiologist. Below are MRI images of the lumbar spine in cross-section. Progressive atrophy is shown from left to right. The multifidus is identified by the white dashed ovals. As the muscle becomes more atrophied the dark muscle is replaced by white fat. This is minimal in the image on the left and is much more pronounced in the image to the far right. The atrophy of important spinal muscles leads to dysfunction and pain.
Instability
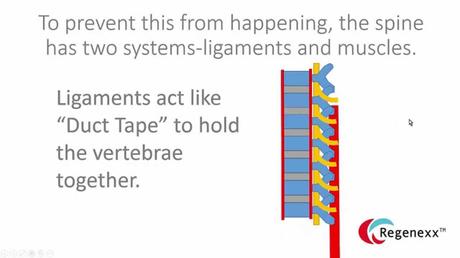
Surgery removes important structures in the spine. Surgery also can compromise ligaments, tendons, and muscles all of which provide important support and stability. Spine surgery typically changes the architecture of the spine which in turn can lead to instability, injury, and pain.
Are there Regenerative Options to Treat Failed Back Surgery Syndrome?
Yes. The Centeno-Schultz Clinic are experts in the evaluation and treatment of low back pain and failed back surgery syndrome. In 2005 we were the first clinic in the world to inject stem cells into the lumbar disc. Treatment options include PRP and a patient’s own bone marrow-derived stem cells. All injections are performed under x-ray or ultrasound guidance or both. Damaged or weakened ligaments can be tightened. Muscles that are atrophied can be injected with PRP to accelerate repair and healing. Injured discs can be injected with both PRP and stem cells to promote healing. Unlike other clinics, we track outcomes that are available here.
In Conclusion
Failed Back Surgery Syndrome is a clinical condition in which patients who have undergone low back surgery continue to have pain and dysfunction. In other words, the surgery failed. Estimates range from 20-40% of patients who undergo low back surgery will develop Failed Back Surgery Syndrome. Pain is the most common symptom of Failed Back Surgery Syndrome. There are a number of reasons for Failed Back Surgery Syndrome which are can be grouped into three major groups: preoperative, postoperative, and diagnostic factors. The best treatment for Failed Back Surgery Syndrome is to AVOID spine surgery. Spinal surgeries do not carry a high success rate. Repeat or revision surgeries are even less successful. Other complications associated with spine surgery include adjacent segment disease, muscle atrophy, and instability. Regenerative options to treat failed back surgery include PRP and bone marrow-derived stem cells.
Know the truth. Spinal surgery is not the answer. Surgeons are biased and advocate for surgical solutions that are not in your best interest. If you or a loved one has ongoing spinal pain please schedule a telemedicine consult with Centeno-Schultz Clinic. Learn from board-certified, fellowship-trained physicians your treatment options. It is time to stop the misery and pain associated with spine surgery.
1.Thomson S. Failed back surgery syndrome – definition, epidemiology and demographics. Br J Pain. 2013;7(1):56-59. doi:10.1177/2049463713479096.
2.Parker SL, Mendenhall SK, Godil SS, et al. Incidence of Low Back Pain After Lumbar Discectomy for Herniated Disc and Its Effect on Patient-reported Outcomes. Clin Orthop Relat Res. 2015;473(6):1988-1999. doi:10.1007/s11999-015-4193-1
3.Daniell JR, Osti OL. Failed Back Surgery Syndrome: A Review Article. Asian Spine J. 2018;12(2):372-379. doi:10.4184/asj.2018.12.2.372
4. Daniell JR, Osti OL. Failed Back Surgery Syndrome: A Review Article. Asian Spine J. 2018;12(2):372-379. doi:10.4184/asj.2018.12.2.372
5. Harris IA, Traeger A, Stanford R, Maher CG, Buchbinder R. Lumbar spine fusion: what is the evidence?. Intern Med J. 2018;48(12):1430-1434. doi:10.1111/imj.14120.
6.Hedlund R, Johansson C, Hägg O, Fritzell P, Tullberg T; Swedish Lumbar Spine Study Group. The long-term outcome of lumbar fusion in the Swedish lumbar spine study. Spine J. 2016;16(5):579-587. doi:10.1016/j.spinee.2015.08.065.
7. Delitto A, Piva SR, Moore CG, Welch WC. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis. Ann Intern Med. 2015;163(5):397-398. doi:10.7326/L15-5129-4.
8. Deyo RA, Hallvik SE, Hildebran C, et al. Use of prescription opioids before and after an operation for chronic pain (lumbar fusion surgery). Pain. 2018;159(6):1147-1154. doi:10.1097/j.pain.0000000000001202
9. Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979-987. Published 2016 Nov 7. doi:10.2147/JPR.S92776.
10. Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976). 2004 Nov 15;29(22):2516-20.
11.Ghiasi MS, Arjmand N, Shirazi-Adl A, et al. Cross-sectional area of human trunk paraspinal muscles before and after posterior lumbar surgery using magnetic resonance imaging. Eur Spine J. 2016;25(3):774-782. doi:10.1007/s00586-015-4014-y

