The headaches, dizziness and brainfog has been unrelenting. They started after a slow speed rear end motor vehicle accident and has been progressive. Physical therapy, medications and rest have failed to provide any benefit. Referrals to specialists including neurologists, orthopedic surgeons and neurosurgeons have been draining and discouraging. Many physicians are dismissive and recommend psychological counseling. My chiropractor believes there is irritation of the brain and may be causing my symptoms.
What is the brainstem and what is its role? What is Cervical Medullary Syndrome? What are the symptoms of Cervical Medullary Syndrome? What are the four major causes of Cervical Medullary Syndrome? How does Craniocervical Instability cause Cervical Medullary Syndrome? Meet Pam. How is Cervical Medullary Syndrome treated? Let’s dig in.
Introduction
Cervical Medullary Syndrome is a clinical condition that occurs as a result of injury to the lower part of the brain.
Important Neck Anatomy
The brain is contained in a protective boney shell called the skull. There are many different parts of the brain. The lowest part of the brain is called the medulla.
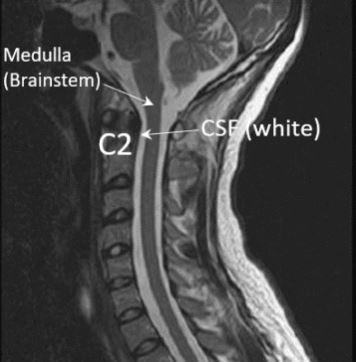
The Medulla is protected and encircled by cerebral spinal fluid. This is illustrated in the sagitial MRI of the brain and neck shown below. This is a side-view image of the anatomy. The Medulla is dark in color and located at the base of the skull. It connects directly with the spinal cord which is also dark in color. The bones of the cervical spine stack one upon another. In contrast the Cerebral Spinal Fluid (CSF) is white in color and that provides an important layer of protection.
There are 7 vertebral bones that make up the cervical spine. They sit in front of the spinal fluid and spinal cord. The second highest bone is the C2 bone and is identified in white.
What Exactly Is Cervical Medullary Syndrome?
Cervical Medullary Syndrome is a clinical condition that occurs as a result inflammation, deformity, or compression of the lower part of the brain (1). Symptoms can be extensive with fluctuating severity based upon the extent of the underlying injury. For example mild irritation of the brainstem may cause only mild, intermittent symptoms.
What Are the Symptoms of Cervical Medullary Syndrome?
Symptoms of cervical medullary syndrome will vary depending upon the severity of the injury. Common symptoms include
- Headache
- Neck pain
- numbness and weakness in the arms, hands, legs
- Dysautonomia
- POTS (postural orthostatic tachycardia syndrome)
- Reduced or loss of breathing
- Visual disturbances
- Problems with Swallowing
- Dizziness
Four Major Conditions that Can Cause Cervical Medullary Syndrome
The upper cervical spine and brain is complex with mulitple structures. These structures reside within the skull and protective confiines of the cerivcal spine. Neither expand to accomodate inflammation, injury and disease. Rather the delicate tissues of the brain and spinal cord are irritated or compressed. The 4 major conditions that cause cervical medullary syndrome are:
Chiari Malformation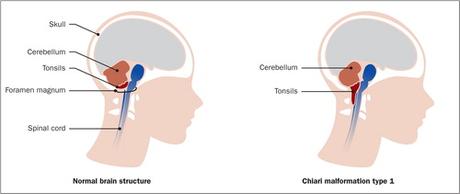
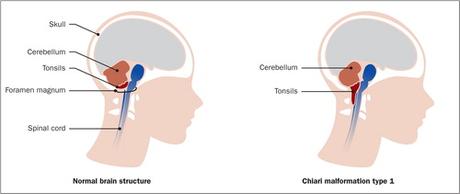
Chiari Malformation is a medical condition where a part of the brain bulges through a normal opening at the base of the skull. To learn more please read my previous blog
Craniocervical Instability
Craniocervical instability (CCI) is a medical condition where the strong ligaments that hold your head onto your upper neck are loose or injured. To learn abou the 7 most common symptoms of CCI plesae click here. To download our newest CCI ebook please click here.
Atlantoaxial Instability
The C1 bone is often times referred to as the atlas. The C2 bone is also called the axis. The C1 and C2 bones stack upon one another forming a joint. The joint is called the atlantoaxial joint (AA). Trauma and ligament instability are the most common causes of Atlantoaxial instability. To learn more about the atlantoaxial joint and its importance please click here.
Cervical Spinal Stenosis
Stenosis simply means narrowing. Cervical spinal stenosis is a medical condition where there is narrowing of the spinal canal which can cause irritation or injury to the spinal cord and nerves resulting in pain, numbness and dysfunction.
How Does Craniocervical Instability (CCI) Cause Cervical Medually Syndrome?
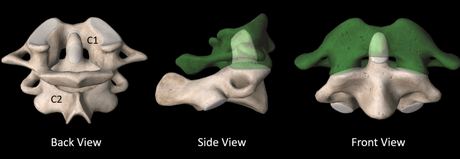
Under normal conditions the C2 bone fits inside the C1 bone as shown above. This enables the C2 to rotate around the C1 bone which is the spot where half of your neck rotation originates.
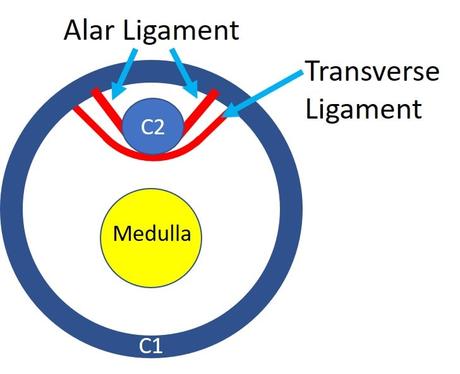
There are two strong ligaments that hold the C2 bone (axis) to the C1 bone (atlas). They are the Alar and Transverse ligaments which are illustrated below. The image is a cross section view from the top down. You know. As if an angel where looking down upon you. The Alar and Transverse ligaments are in red and snuggly hold the top of the C2 bone into place. Behind the C2 bone is the cerebral spinal fluid along with the brainstem (Medulla). The cerebral spinal fluid is white in color whereas the brainstem is yellow. The Alar and Transverse ligaments snuggly holds the C2 bone preventing it from striking or injuring the medulla.
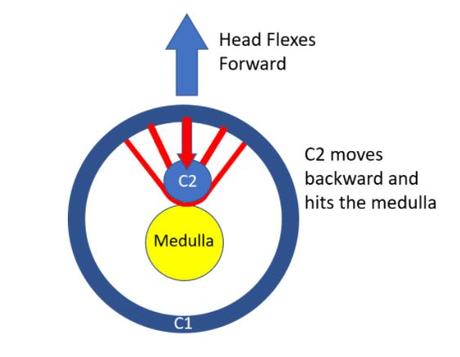
Now let’s look at what happens with patients that have Craniocervical instability (CCI). This is a condition where there is injury or damage of the alar and or transverse ligaments. This is illustrated below. Because the alar and transverse ligaments are loose the C2 bone is no longer held snuggly into place. Rather it is moves backwards and contacts the medulla when a patient bends their head and neck. The protective cerebral spinal fluid is displaced and is no longer able to act as a buffer. The medulla is very, very sensitive tissue which is easily irritated or compressed by the C2 bone. This gives rise to symptoms of cervical medullar syndrome.
Meet Pam
Pam is 50 y/o patient evaluated in clinic with a 4 year history of brain fog, headaches, memory problems, fatigue and visual disturbances. She was enjoyed gynamistics and cheerleading in high school and considered herself very flexible. She had history mutliple small trauma due to sports. Symptoms were severly aggravated by motor vehicle accident. She was evaluated by a number of specialists including neurologists, orthopedic surgerons and neurosurgeon without a clear explanation of the symptms. The traditional MRI studies were “normal”.
An upright flexion/ extension MRI clearly demonstrated the problem. The side view section of Pam’s MRI is shown below. it demonstrates what is happening when Pam bends her head and neck forward.

The C2 bone is identified by a the yellow triangle. The brainstem is black in color, tubular in structure and immediately behind the C2 bone. It is a continuation of the brain and connects to the spinal cord. It is a fragile tissue that is susceptible to irritation, inflammation and injury. Cerebral spinal fluid provides important protection for the Brainstem and spinal cord. It is white in color and surrounds the Brainstem and spinal cord. Unfortunately in Pam’s case when she bends her head forward that protective layer is not logner present. Rather her Brainstem strikes the backside of the C2 bone causing her symtpoms. Ouch!
How Is Cervical Medullary Syndrome Treated?
The first-line treatment is often physical therapy or specific upper cervical chiropractic. In our experience, the latter is usually more successful in some patients, as it more directly addresses the malposition of C1 on C2, which tend to rotate on each other when there are loose or damaged ligaments. When this doesn’t help, a surgical Fusion of the upper neck bones is usually recommended. This involves using screws and sometimes plates or rods to make sure the upper neck bones don’t move. However, this is a high-risk procedure that can’t be undone. In addition, it can also cause Adjacent Segment Disease (ASD), which means that the spinal levels above and below can get worn out and damaged, requiring the need for more Fusions.
An alternative is trying to tighten the ligaments through very specific x-ray guided injections. While prolotherapy (ligament tightening injections) on the ligaments in the back of the neck can be tried, the ligaments discussed here that cause the Cervical Medullary Syndrome can’t be reached or treated using that method. The PICL procedure does treat these ligaments directly. The procedure is only performed at the Centeno-Schultz Clinic in Brommfield Colorado. To learn more about the Percutaneous Implantation of CCJ Ligaments please click on the video below.
In Conclusion
Cervical Medullary Syndrome is a clinical condition that occurs as a result inflammation, deformity, or compression of the lower part of the brain.
There are numerous symptoms with fluctuating severity based uon the extent of the underlying injury.
The most common symptoms of Cervical Medullary Syndrome include headache, neck pain, numbness and weakness in the arms, hands and leg, dysautonomia, visual disturbances and dizziness.
The four most common conditions that cause Cervical Medullary Syndrome are:
- Chiari Malformations
- Craniocervical Instability
- Atlantoaxial Instability
- Cervical Spinal Stenosis
First line treatment when appropriate is physical therapy and chiropractic care. When conservative treatment options fail surgery is often recommended in the form of a Fusion.
Tightening and strengthening the Alar and Transverse ligament is now possible through the PICL procedure.
The PICL is a non-surgical treatment.
If you or a loved one have ongoing neck pain, headache, and dizziness that has not responded to conservative treatment, please schedule a telephone Candidacy discussion with a board-certified, fellowship-trained physician. At the Centeno-Schultz Clinic, we are experts in the evaluation and treatment of upper neck injuries. From the comfort of your home or office learn what treatment options are available for you.
1.Henderson FC Sr, Francomano CA, Koby M, Tuchman K, Adcock J, Patel S. Cervical medullary syndrome secondary to craniocervical instability and ventral brainstem compression in hereditary hypermobility connective tissue disorders: 5-year follow-up after craniocervical reduction, fusion, and stabilization. Neurosurg Rev. 2019;42(4):915-936. doi:10.1007/s10143-018-01070-4

