It was all a blur. The headaches, brain fog and fatigue started gradually and got worse. Simple tasks became overwhelming. Isolation and functional limitation ensued. Physical therapy, chiropractic care, medications and rest failed to help. Physicians were not certain as to the cause of my symptoms. Many were dismissive and suggested that it was an emotional or pyschological issue. Your chiropractor thought the problem was in your neck. What is Craniocervical Instability? What are the eight most common symptoms of Craniocervical Instability? How is Craniocervical Instability Diagnosed? What are the treatment options for Craniocervical Instability? What is Craniocervical Instability Surgery? What non-surgical treatment options exist? Meet AW. Let’s dig in.
What Is Craniocervical Instability?
Cranial Cervical Instability (CCI) is a medical condition where the strong ligaments that hold your head to your upper neck are loose or lax (1). The major ligaments involved are the Alar, Transverse and Accessory ligaments. To learn more about CCI please click on the video below.
What Are the Eight Most Common Symptoms of Craniocervical Instability?
Excessive movement between your head and neck can irritation and damage of the upper cervical facet joints, discs, nerves, and blood vessels. Symptoms vary depending upon the amount of instability. The most common symptoms include:
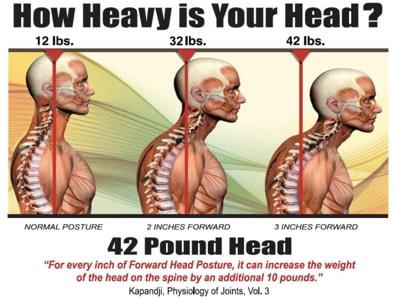
1. Painful, Heavy Head
A constant to near-constant head pain can be described as feeling like the head is too heavy for the neck to support. Many describe feeling like they have a “bobblehead”. Neck weakness along with ligament instability results in head forward posture in many patients. This has significant consequences as the weight of your head dramatically increases as it moves forward from neutral alignment. This is illustrated below. On the left, in neutral spinal alignment, your head weighs 12 lbs. With just 2 inches forward posture the weight of the head increases to 32lbs. Add another 1 inch forward and the weight increases to 42lbs. This is an enormous amount of weight that can not be sustained or supported. Often times the result is chronically tight trap muscles as they are now tasked with supporting this heavy head.
2. Headache
This is not your normal headache caused by your in-laws or excessive consumption of alcohol. This is a debilitating headache that is constant in duration and miserable. The headache may be localized at the base of the skull (suboccipital) or radiate from the upper neck into the forehead and eyes in a ram’s horn distribution.
3. Brain Fog

Patients with CCI can struggle with memory, concentration, and ability to complete tasks. Every day can feel like your brain is stuffed full of cotton. Executive function can be severely compromised making employment or studying nearly impossible.
4. Rapid Heart Rate
Elevated heart rate may occur as the vagus nerve gets irritated by the extra motion in the upper neck. Another cause of elevated heart rate is Postural Orthostatic Tachycardia Syndrome (POTS). POTS is a medical condition that causes malfunction of the autonomic nervous system. It is estimated to impact between 1,000,000 and 3,000,000 Americans. The autonomic nervous system controls involuntary body functions such as heart rate and blood pressure. Malfunction of the autonomic nervous system causes several symptoms which include rapid heart rate.
5. Neck Pain
Neck pain is typically localized at the base of the skull and aggravated with flexion,rotation and lateral side bending. The pain be localized or radiate up into the base of the skull causing a headache. The pain can also radiate down into the lower neck and shoulders causing trapezius and scapular pain. Neck pain can be sharp and stabbing, dull and aching or throbbing.
6. Visual Problems
Visual disturbances can vary from mild to severe involving a number of symptoms. Visual disturbances can happen because the upper neck supplies information to the brain to guide eye position and vice versa (2).
How Is Craniocervical Instability Diagnosed? 7 Main Criteria
At the Centeno-Schultz Clinic we are committed to understanding and identifying the underlying cause of your pain and dysfunction. For that a correct diagnosis must be made. Treating symptoms is helpful but does not provide for the best clinical outcome. Craniocervical Instability is poorly understood and often times missed. Diagnosing Craniocervical Instability involves 7 main criteria which include:
1. Mechanism of Injury (How Did It Occur)

Understanding how and when the injury occurred is important. The two most common causes of Cranial Cervical Instability (CCI) are trauma and medical conditions that cause people to have loose or compromised ligaments (2). Motor vehicle accidents, contact sports, and forceful manipulations by chiropractors are the most common examples of trauma. Ehlers Danlos Syndrome (EDS) is a group of inherited disorders that affect your ligaments and connective tissues (2).
2.Symptoms
The symptoms associated with CCI can be extensive depending upon the severity of the instability. The most common symptoms were described above.
3.Physical Examination
In the age of managed care and 15-minute appointments, the art and practice of physical examination by a physician is almost gone. At the Centeno -Schultz Clinic all new patient evaluations undergo an extensive physical examination. Why? It is important to view the body as a whole and there are multiple potential physical findings in the neck, head, shoulder, and low back in patients with Cranial Cervical Instability,
4. Radiographic Studies
There are various types of radiographic studies which include x-ray, CT scan, and MRI. Unfortunately, traditional MRI and CT studies do not evaluate the upper cervical spine or Alar and Transverse ligaments. Special radiographic studies are required which include upper cervical MRI or rotatory CT scan. In addition, there are additional studies that involve the patient moving during the examination. These dynamic studies are useful to identify instability. Examples include upright MRI with upright flexion/extension. To see how this works please click on the video below.
Finally, a Digital Motion X-ray (DMX) study is important in establishing the diagnosis of CCI. This is an x-ray examination that is recorded in which the patient is put through various movements including bending the neck forward, backward, and to the side. To learn more about DMX please click on the video below.
5. Response to Conservative Care
The common symptoms of CCI can also arise from different clinical conditions. For example, headaches with dizziness may arise from tight or contracted neck muscles. It is important that patients undergo conservative care such as rest, heat, stretching, physical therapy, massage, and chiropractic care. In some cases, symptoms improve with conservative therapy.
6. Response to Diagnostic Injections
A diagnostic injection is a precise injection into a specific structure asking the question of whether or not it resolved the pain. Often times this is very helpful in the evaluation of patients with CCI. All diagnostic injections are performed under ultrasound or x-ray or both. Examples of diagnostic injections include cervical facets, occipital nerve blocks and ligament injections.
7. Level of Disability
In many cases due to the severity of the symptoms patients are not able to complete their domestic or professional responsibilities. In severe cases of CCI, patients are confined to their homes and are socially isolated. The level of disability is important in diagnosing Craniocervical Instability (CCI).
Craniocervical Instability Treatment Options: Conservative Care, Injections and Surgery
Treatment of Craniocervical Instability is challenging. Not having an accurate diagnosis can make it even more challenging. A lack of diagnosis can send patients on a many-year journey looking for assistance. Some will be dismissed as their complaints are considered not valid or genuine whereas others will be labeled “hormonal”, anxious or psychiatric and referred elsewhere or medicated with anti-depressants, opioids, or anti-anxiety medications. There are three major types of CCI treatments: conservative care, injections and Craniocervical Instability Surgery. The specific type of treatment will depend upon the amount of instability and a patient’s clinical presentation.
Conservative Care
Patients with small amounts of instability can oftentimes be managed with conservative care. Treatment options include:
1. Upper cervical chiropractic care. Look for members of NUCCA (National Upper Cervical Chiropractic Association)
2. Physical Therapy
3. Bracing
4. Curve restoration. Look for chiropractors that specialize: Chiropractic BioPhysics or CBP is a protocol utilized by a select group of chiropractors who look to spinal rehabilitation and postural correction as a means to address pain, disease, and dysfunction.
Precise Injections
Precise x-ray guided injections with PRP or bone marrow concentrate which contains stem cells are the next treatment options for those patients who fail to receive any clinical benefit from conservative care. Examples include
- C0/1 and C1/2 facet injections. A facet is a paired joint on the backside of the spine that provides support and limits rotation of the spine. It can also be irritated or injured causing significant neck and head pain (3). Few clinics perform this injection due to the skill required.
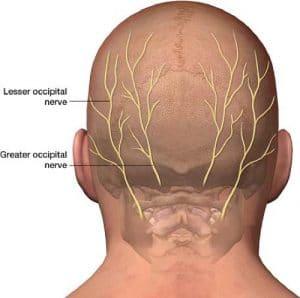
- Occipitals Nerve block. The Occipital nerves arise from the upper cervical spine and travel up into the back of the head. There is one nerve on each side of the head. When irritated, injured, or compressed they can cause significant pain in the back and top of the head (4).
- Superficial Cervical Plexus injection
- Ligament injections to stabilize injured or lax ligaments. Ligaments are thick pieces of connective tissue that connect bone to bone. Loose or damaged ligaments can cause significant instability, pain, and dysfunction.
Surgery
Craniocervical Instability Surgery always involves a fusion. Fusion is a surgical procedure where one or more of the bones in the spine are joined together by screws, bolts, and rods. The hardware provides mechanical stability. In most cases of Craniocervical Instability, the upper portion of the neck (C1 and C2 vertebral bodies) is fused to the skull. The skull is also called the occiput. The surgery can also be called an Occipitocervical Fusion. This is major surgery and rehabilitation. The procedure depending upon the complexity typically ranges from 130-320 minutes (9).
The upper cervical spine is a very complex area rich in nerves, arteries, veins, ligaments, tendons, and muscles. The risks associated with upper neck fusion are significant and include (9):
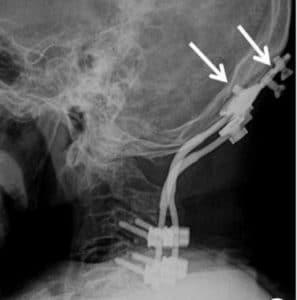
Screw failure: The screw that is inserted into the occiput or C1 or C2 can fracture, bend or break. In most cases surgical revision is necessary.
Screw loosening: The implanted screw can back out of the bone over time compromising the stability of the upper neck.
Infection: The infection can be localized to the skin or may penetrate deeper into the muscles or bone. Antibiotics are oftentimes required for skin infections. Bone infections require additional surgery.
Vertebral Artery injury: The Vertebral Artery provides critical blood flow to the spinal cord and brain. The artery can be compressed, irritated, or injured during the surgery.
Spinal Cord Injury: The spinal cord runs from the base of the head to the lower back and contains critical nerve tissue that controls the central nervous system.
Cervical Facet Injury: The screw can be advanced into the facet joint thereby injuring the joint cartilage leading to arthritis, pain, and restriction in range of motion.
Upper Neck Muscle Weakness: The muscles can be injured during surgical fusion.
Dural Leak: The Dura is a thin layer of connective tissue that covers the brain and spinal cord. It can be injured during the surgery resulting in leakage of spinal fluid (10).
Hematoma: A collection of blood that can compress or injure nerves, arteries, and veins
Persistent upper cervical instability requiring additional surgery .(11)
Limited Neck Range of Motion: Fusion of the skull base to the upper neck can severely restrict the range of motion in the upper neck.
Adjacent Segment Disease ( ASD): Fusion of the spine significantly alters the biomechanics of the spine. The fused segment is no longer able to absorb the forces of daily living. As such these forces are then transferred above and below the fusion. This additional force can overload the discs, facet joints, muscle, and ligaments above and below the fusion which start to break down. To learn more about Adjacent Segment Disease please click on the video below.
A New Nonsurgical Regnerative Treatment Option: The “PICL”
In 2015 a nonsurgical treatment option for Cranial Cervical Instability was developed at the Centeno-Schultz Clinic. It involves the injection of a patient’s own bone marrow concentrate which contains stem cells into the damaged Alar and Transverse ligaments. The procedure is very demanding and only performed at the Centeno-Schultz Clinic in Broomfield Colorado. The procedure is called Percutaneous Implantation of Cervical Ligaments (PICL) To learn more about this groundbreaking procedure please click on the video below.
Meet AW: Another PICL Success Story
AW is a 29 y/o athletic Denver travel agent who presented with a 5-year history of neck pain and neurologic symptoms. Her past medical history was significant for hypermobility and chronic fatigue. Her neck pain was constant involving her entire neck with radiations into her head with debilitating headaches. Her neurologic symptoms included brain fog, headaches, nausea, dizziness and heavy head and difficulty swallowing. Onset of symptoms was not associated with trauma. Physical therapy, rest, medications, acupuncture, heat, ice, stretching, chiropractic failed to provide any relief. AW was evaluated by multiple physicians without a clear diagnosis. Focus was placed on treating symptoms as opposed to understandin the underlying problem. Her history together, physical examination and abnormal Digital Motion X-ray confirmed the diagnosis of craniocervical instability. She declined fusion surgery and proceeded with two PICL procedures where bone marrow concentrate containing stem cells was injected directly into the damaged cervical ligaments. Her response has been dramatic. AW summarizes her journey and results from the PICL procedures best:
“It’s been 5 years since I had to change careers and take a desk job, and 4 years since I was housebound due to my then diagnosis of Chronic Fatigue Syndrome. Before finally finding Dr. Schultz, I had seen 27 specialists and doctors, none of whom had any idea how to help a previously strong and healthy 25 year-old who went from playing club volleyball at CU Boulder and hiking daily to having to be carried to her home office from bed everyday. To say it’s been a long and painful road is an unbelievable understatement, but after being accurately diagnosed by Dr. Shcultz with CCI in Feb 2021 and treated with two PICL procedures, I am now recovering and living life again, rather than managing my symptoms. Not only am I able to walk to my desk and work a full day, I was able to take long walks on the sandy beaches in Hawaii last week, fly to Hawaii in the first place, snorkel for hours, and just went on my first hike in more than 5 years in Steamboat this weekend. I can’t even begin to describe how incredibly thankful I am for Dr Schultz and his team, the procedure, and for the many now possible adventures to come. “
In Conclusion
- Craniocervical Instability is a medical condition characterized by injury and instability of the ligaments that hold your head onto the neck.
- Common symptoms of Cranial Cervical Instability include a painful, heavy head, headache, rapid heart rate, brain fog, neck pain, visual problems, dizziness, and chronic fatigue.
- CCI or neck ligament laxity treatment options depend upon the severity of the instability and clinical symptoms. When appropriate, conservative care should always be the first-line treatment.
- Craniocervical Instability Surgery is often recommended when conservative care fails. This involves a fusion of the head to the neck which is a major surgery that is associated with significant risks and complications.
- The PICL procedure is a revolutionary non-surgical Craniocervical Instability treatment option where a patient’s own stem cells are injected into the damaged upper cervical ligaments.
- AW successfully avoided Craniocervical Instability surgery by having her stem cells injected into her damaged Alar and Transverse ligaments at the Centeno-Schultz Clinic.
If you or a loved one has sustained an injury with ongoing headaches, neck pain, and brain fog please schedule a telephone candidacy discussion with a board-certified, fellowship-trained physician. From the comfort of your home or office learn what treatment options are available for you. Call today and stop the pain, misery, and suffering.
1.Offiah CE, Day E. The craniocervical junction: embryology, anatomy, biomechanics and imaging in blunt trauma. Insights Imaging. 2017;8(1):29–47. doi:10.1007/s13244-016-0530-5
2.Sobey G. Ehlers-Danlos syndrome – a commonly misunderstood group of conditions. Clin Med (Lond). 2014;14(4):432-436. doi:10.7861/clinmedicine.14-4-432
3.Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004;5:15. Published 2004 May 28. doi:10.1186/1471-2474-5-15
4.Juškys R, Šustickas G. Effectiveness of treatment of occipital neuralgia using the nerve block technique: a prospective analysis of 44 patients. Acta Med Litu. 2018;25(2):53-60. doi:10.6001/actamedica.v25i2.3757
5. Mazur MD, Ravindra VM, Brockmeyer DL. Unilateral fixation for treatment of occipitocervical instability in children with congenital vertebral anomalies of the craniocervical junction. Neurosurg Focus. 2015 Apr;38(4):E9. doi: 10.3171/2015.1.FOCUS14787. PMID: 25828503..

