Your thumb pain is debilitating. Opening a jar is almost impossible. Your doctor thinks your CMC joint is injured. What is the CMC joint? What are the 5 most common sources of CMC joint Pain? What is CMC joint osteoarthritis? What causes it? What are the symptoms of CMC joint arthritis? How is CMC joint arthritis diagnosed? What factors affect the stability of the CMC joint? What are the treatment options? What are the complications associated with CMC joint surgery? Are there effective non-surgical treatment alternatives? Let’s dig in.
What Is the CMC Joint? (Thumb Joint)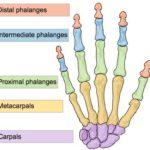
The hand is composed of 27 bones that can be divided into two major groups. The carpal and metacarpal bones. They are illustrated to the right.
The thumb is also referred to as the CMC joint. It is composed of two bones. The Carpal bone is denoted by the letter C. The second bone, the MC is the MetaCarpal bone. So your thumb is made up of the Carpal and MetaCarpal bones that come together and form a joint. The joint is lined with cartilage which allows the two bones to slide smoothly against one another. The thumb joint is held together by multiple thick ligaments. Ligaments are thick pieces of connective tissue that connect one bone to another. This joint is a saddle-shaped joint that experiences significant forces through activities of daily living. For example, think of the forces required to open a stubborn jar. These forces along with the unique shape make the CMC joint vulnerable to injury (1).
What Are the 5 Major Causes of CMC Joint Pain? (Thumb Pain)
Thumb pain can be debilitating making simple daily chores almost impossible. Common causes of thumb pain include:
Osteoarthritis
Up to 15% of the population older than 30 years suffers from CMC joint arthritis (2). In patients older than 75 years, thumb arthritis has a prevalence of 25% in men and 49% in women. For more information please see the section below.
Fracture
A fracture can occur in the carpal or metacarpal bone. Direct stress, such as from a fall is the most common cause. CMC fractures account for 4% of all hand fractures (3).
Tendon Injuries
Tendons are thick pieces of connective tissue that connect muscle to bone. There are a large number of tendons in the wrist, hand, and thumb. Inflammation, injury, or degeneration of a tendon can cause CMC joint pain. De Quervains tendonitis is a common condition among young mothers and video game enthusiasts that involves inflammation of wrist tendons. It can present as thumb pain. To learn more click here.
Ligament Injuries
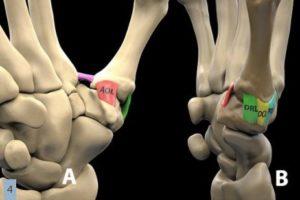
Ligaments of the CMC Joint
Ligaments are thick pieces of connective tissue that connect bone to bone. The thumb has a large number of ligaments that provide important support for the CMC joint. The most important ligament is the anterior oblique ligament (AOL) pictured below. Also known as the “beak ligament” connects the carpal bone to the metacarpal bone. Injury or laxity of the ligaments is a major contributor to osteoarthritis and CMC joint pain (4).
Nerve Injury
Nerves can become irritated or injured causing pain. Carpal Tunnel Syndrome is a common medical condition and involves compression of the median nerve at the level of the wrist (5). Symptoms include weakness, tingling, burning, and CMC joint pain. To learn more about Carpal Tunnel Syndrome and treatment options click here.
What Is CMC Joint Osteoarthritis? (Thumb Arthritis)
Osteoarthritis is the most common form of arthritis affecting over 32 million U.S adults annually. It involves the gradual breakdown and erosion of the joint cartilage. It occurs most frequently in the hands, hips, and knees. CMC joint osteoarthritis is a chronic, painful condition that involves the breakdown of the cartilage in the thumb. CMC joint osteoarthritis has 4 major stages based on severity. This is illustrated in the x-rays to the right (6).

Thumb x-rays illustrating progressive CMC joint arthritis
Stage 1: Subtle thumb space widening. Image A.
Stage 2: Subtle thumb space narrowing, bone spurs, and loose bodies < 2mm. Image B.
Stage 3: Advanced thumb space narrowing, bone spurs, and loose bodies > 2mm
Stage 4: Advanced thumb space narrowing, bone spurs, loose bodies, and arthritis in the neighboring hand joints. Image D
What Causes CMC Joint Arthritis? (Continued Wear & Tear)
CMC joint arthritis is caused principally by many years of using the hand and thumb. Some refer to it as “wear and tear” type arthritis. This condition may be more likely if you have, do, or are:
- Regular, repetitive stress on thumb joint
- History of prior thumb surgery
- History of loose or damaged ligaments
- Misalignment of the thumb bones
- Women and past menopause (7)
- History of hypermobility such as patients with EDS
- Advanced age
- Family history (8)
- Smoking (8)
To learn more about CMC joint arthritis please click here.
What Are the Symptoms of CMC Joint Osteoarthritis? (Pain)
CMC joint osteoarthritis can cause a number of different symptoms. The most common include.
 Thumb Pain
Thumb Pain

Pain is the most common symptom and is typically located at the base of the thumb. It can be intermittent or constant. It is aggravated by gripping, grasping, and pinching activities.
Thumb Weakness
Loss of thumb strength is common. Unscrewing jar tops or turning doorknobs can be almost impossible.
Swelling
The CMC joint can become swollen and red after repetitive activities.
Popping and Grinding
Movement of the CMC joint oftentimes causes audible popping and grinding
Reduced Range of Motion
Loss of cartilage, laxity of the ligament, bone spurs, and muscle weakness cause reduced range of motion in the CMC joint.
How Is CMC Joint Arthritis Diagnosed? (Physical Exam)
A detailed history and physical examination are essential and typically all that is needed for the diagnosis of CMC joint arthritis. On examination, the CMC joint is oftentimes tender to the touch. A reduced range of motion is common. Special maneuvers such as the “grind” test are often performed (9).
X-rays are useful as they will identify areas of arthritis and misalignment. There are 4 distinct stages of CMC joint arthritis based upon the severity of arthritis.
Ultrasound is a powerful diagnostic tool. It can assess the joint space and cartilage and therefore the severity of the CMC joint arthritis. It can also evaluate the ligaments and stability of the joint.
What Factors Affect the Stability of the CMC Joint? (Ligaments)
The stability of the CMC joint is dependent upon two principal factors.
Ligaments
There are a large number of ligaments in the thumb. Ligaments are thick pieces of connective tissue that connect one bone to another. If injured, stretched, or weakened the CMC joint can become unstable. The results in additional movement of the carpal and metacarpal bones. It is similar to the lug nuts on your car’s wheel. If the lug nuts are loose there is additional movement in the wheel and tire. This additional movement results in abnormal wear and tear in the tire tread and a shortened tread life. So too with the CMC joint. Injured, stretched, or damaged thumb ligaments lead to instability which in turn leads to additional CMC joint injuries including arthritis, tendon, and ligament problems.
At the Centeno-Schultz Clinic, we utilize ultrasound guidance to evaluate and treat CMC joint pain. To see an ultrasound of the thumb joint please click on the video below. The carpal bone is in the middle whereas the metacarpal bone is to the right in this video.

Muscles 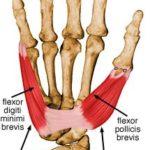
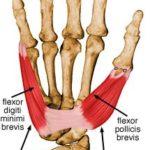
There are multiple small muscles in the thumb and wrist. Muscles keep the thumb and wrist bones in alignment. In doing so they provide important support for the CMC joint. Muscle weakness can lead to CMC joint instability. Common causes of muscle weakness include neuromuscular disorders such as multiple sclerosis, thyroid disease, electrolyte imbalances, peripheral neuropathy, and bulging or herniation of discs in the neck. At the Centeno-Schultz Clinic patients with CMC joint arthritis routinely have a neck x-ray to evaluate possible neck injuries that may be contributing to CMC joint pain. To learn more about the connection between the neck and CMC joint pain please click here.
Treatment for CMC Joint Osteoarthritis
Osteoarthritis is a chronic, progressive condition. Treatment typically focuses on managing symptoms. Treatment varies and is dependent upon the severity of the injury and current symptoms. The three principal treatments for CMC joint pain are conservative care, steroid injections, and surgery.
Conservative Treatment
When appropriate first-line treatment should be conservative therapy. Options include NSAID’s, heat, ice, bracing, low dose narcotics, physical and occupational therapy, acupuncture, and chiropractic care.
Steroid Injections
If conservative treatment fails patients are oftentimes referred for steroid injections. Steroids are powerful anti-inflammatory agents but also have significant side effects which injury to the ligaments and cartilage. Because of their negative side effects, steroid injections for CMC joint pain should be avoided.
Surgery
There are many surgical techniques available to treat CMC joint pain and arthritis when conservative measures have failed (10). Options include shaving one or more of the CMC joint bones which is called an osteotomy. Surgeons can also remove a bone which typically involves the trapezium bone (11). Ligament reconstruction is helpful for those individuals with no cartilage loss. For advanced CMC joint arthritis orthopedic surgeons often times recommend total joint replacement or fusion.
To learn more about CMC joint anatomy and the sources of CMC joint pain please click on the video below.
What Are the Complications Associated with CMC Joint Surgery?
Complications exist and vary depending upon the severity of the underlying CMC joint arthritis, co-existing health problems, and the specific surgery (12). Complications include:
- Bleeding
- Infection
- Nerve Injury
- Complex Regional Pain Syndrome
- Pain
- Swelling
Alternatives to Thumb Surgery
At the Centeno-Schultz Clinic, we are experts in the non-surgical treatment of thumb pain. Treatment options include PRP, bone marrow-derived stem cells, and adipose grafts. PRP stands for platelet-rich plasma which is rich in growth factors that can increase blood flow and decrease inflammation. Stem cells accelerate healing by recruiting local and remote repair cells. Our results are impressive and can be reviewed by clicking here.
We have also published our results using a patient’s own bone marrow-derived stem cells to treat thumb pain and arthritis (13). The results are noteworthy as patients noted an increase both in strength and range of motion after stem cell injections.
The procedures are challenging and can not be performed by your PCP or orthopedic surgeon. To watch an ultrasound-guided hand and thumb injection at the Centeno-Schultz Clinic please click on the video below.

In Conclusion
The thumb is also known as the CMC joint. It is where the Carpal bone meets the Metacarpal bone to form a joint. The 5 major causes of CMC joint pain include osteoarthritis, fractures, tendon injuries, ligament injuries, and nerve problems. Thumb osteoarthritis is common and involves the breakdown of the joint cartilage. There are 4 distinct stages based upon severity. CMC joint arthritis is due to continued wear and tear of the thumb. Risk factors include repetitive stress on the joint, history of prior thumb surgery, loose or damaged ligaments, history of hypermobility, advanced age, family history, smoking, and female gender who are postmenopausal. The most common symptoms of CMC joint osteoarthritis include thumb pain, weakness, swelling, popping and grinding, and reduced range of motion. CMC joint osteoarthritis is diagnosed by history, physical examination, and x-rays. Ligaments and muscles are the two key factors that affect joint stability in the thumb. Treatment options for CMC joint osteoarthritis include conservative care, steroid injections, and surgery. Steroids are toxic to cartilage and supporting ligaments and should be avoided. Many different types of surgery exist and include shaving bones, removing bones, ligament reconstruction, joint replacement, and fusion. Surgical complications include bleeding, infection, nerve injury, pain, and swelling.
PRP and stem cells are effective alternatives to both surgery and steroid injections. The Centeno-Schultz Clinic are experts in the treatment of CMC joint pain. Our outcomes are all tracked and we have published our results. PRP and stem cells allow patients to use the healing power inherent in their own bodies and avoid the complications associated with steroid injections and surgery.
If you or a loved one suffers from thumb pain please schedule a telemedicine consultation to learn about the best treatment options. From the comfort of your own home, backyard, or cabin speak with a board-certified, fellowship-trained physician who can review your history and radiographic studies. Thumb pain is a warning sign that you have a problem that warrants investigation. Thumb pain left untreated typically get worse with an escalation in pain and reduced motion. Don’t risk dependence on NSIAD or narcotics. Stop the suffering and schedule today.
1. Higgenbotham C, Boyd A, Busch M, Heaton D, Trumble T. Optimal management of thumb basal joint arthritis: challenges and solutions. Orthop Res Rev. 2017;9:93-99. Published 2017 Nov 23. doi:10.2147/ORR.S138809
2.Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study [published correction appears in Ann Rheum Dis. 2018 Oct;77(10):1546]. Ann Rheum Dis. 2011;70(9):1581-1586. doi:10.1136/ard.2011.150078
3. .Stanton JS, Dias JJ, Burke FD. Fractures of the tubular bones of the hand. J Hand Surg Eur Vol. 2007 Dec;32(6):626-36. doi: 10.1016/J.JHSE.2007.06.017. Epub 2007 Sep 21. PMID: 17993422.
4. Gillis J, Calder K, Williams J. Review of thumb carpometacarpal arthritis classification, treatment and outcomes. Can J Plast Surg. 2011;19(4):134-138. doi:10.1177/229255031101900409
5.Genova A, Dix O, Saefan A, Thakur M, Hassan A. Carpal Tunnel Syndrome: A Review of Literature. Cureus. 2020;12(3):e7333. Published 2020 Mar 19. doi:10.7759/cureus.7333
6. Kennedy CD, Manske MC, Huang JI. Classifications in Brief: The Eaton-Littler Classification of Thumb Carpometacarpal Joint Arthrosis. Clin Orthop Relat Res. 2016;474(12):2729-2733. doi:10.1007/s11999-016-4864-6
7.Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study [published correction appears in Ann Rheum Dis. 2018 Oct;77(10):1546]. Ann Rheum Dis. 2011;70(9):1581–1586. doi:10.1136/ard.2011.150078
8. Fontana L, Neel S, Claise JM, Ughetto S, Catilina P. Osteoarthritis of the thumb carpometacarpal joint in women and occupational risk factors: a case-control study. J Hand Surg Am. 2007 Apr;32(4):459-65. doi: 10.1016/j.jhsa.2007.01.014. PMID: 17398355.
9.Burton RI. Basal joint arthrosis of the thumb. Orthop Clin North Am. 1973 Apr;4(2):331-8. PMID: 4707436.
10. Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984 Sep;9(5):692-99. doi: 10.1016/s0363-5023(84)80015-5. PMID: 6491213.
11.Gervis WH. Excision of the trapezium for osteoarthritis of the trapezio‐metacarpal joint. Journal of Bone & Joint Surgery 1949;31(4):357‐9. https://www.ncbi.nlm.nih.gov/pubmed/15397137.
12. Naram A, Lyons K, Rothkopf DM, et al. Increased Complications in Trapeziectomy With Ligament Reconstruction and Tendon Interposition Compared With Trapeziectomy Alone. Hand (N Y). 2016;11(1):78-82. doi:10.1177/1558944715617215
13. Centeno CJ, Freeman MD. Percutaneous injection of autologous, culture-expanded mesenchymal stem cells into carpometacarpal hand joints: a case series with an untreated comparison group. Wien Med Wochenschr. 2014 Mar;164(5-6):83-7. doi: 10.1007/s10354-013-0222-4. Epub 2013 Aug 15. PMID: 23949564.

