You hear it as you walk down the stairs. The clicking in your knee is increasing! Your PCP simply dismisses it as part of aging but you are concerned. What are the major causes of clicking in the knee? When should I be concerned about clicking in the knee? How do I get my knee to stop clicking? Let’s dig in.
5 Major Causes of Clicking in Knee

Major Knee Ligaments
Clicking in knee can occur for a number of reasons. The 5 major causes include:
Ligament Injuries
A ligament is a thick piece of connective tissue that connects one bone to another. The knee has 4 principal ligaments: ACL, PCL, MCL, and LCL. Ligaments provide important stability for the knee (1). If injured or torn, ligaments can create instability. This instability can cause clicking in the knee. As ligaments travel across boney surfaces they can also catch causing a clicking in the knee.
Meniscus Tear
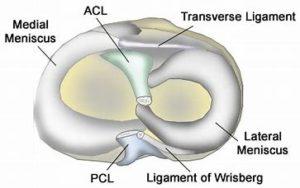
Cross Section Knee Meniscus
The meniscus is a C shaped cushion situated between the thigh bone and shin bone. Each of us has two menisci per knee. One on the inside (medial) and one of the outside (lateral) of the knee. The meniscus functions as a shock absorber and joint stabilizer and is susceptible to injury. Meniscus tears are among the most common knee injuries. There are many different types of meniscus tears that are classified (2). Examples include horizontal, vertical, and complex Risk factors for meniscus tears include advanced age, male gender, work-related kneeling, and climbing stairs (3). Injury to the meniscus can cause clicking in the knee that is often times associated with pain.
Osteoarthritis
Osteoarthritis is the most common form of arthritis. It is a joint disease where the cartilage that lines and protects the joint gradually wears down resulting in pain, swelling, and restriction in movement. Approximately 13% of women and 10% of men aged 60 years and older have symptomatic knee osteoarthritis (4). Risk factors for knee osteoarthritis include obesity, female gender, repetitive knee trauma, muscle weakness, squatting, and meniscus injuries (5). Loss of cartilage and knee swelling can cause clicking in the knee.
Patellofemoral Syndrome
Patellofemoral syndrome, also known as runner’s knee is a medical condition where there is a misalignment of the kneecap. The kneecap is intended to smoothly glide up and down a boney groove in the thigh bone. The thigh bone is also known as the femur. The knee cap is sometimes called the patella. In patellofemoral syndrome, the knee cap no longer tracks smoothly in the boney groove. As a result of misalignment, the knee cap rubs repetitively against the boney wall with injury to the cartilage, ligaments, and tendons. These injuries oftentimes result in clicking in the knee and or, pain and swelling.
Soft Tissue/Scar Tissue
Surgery or significant trauma can cause soft tissue in the knee to become injured and inflamed. In addition, scar tissue can also develop. Both soft tissue injury and scar tissue can cause clicking in the knee. Clicking in the knee is extremely common during the first year after knee surgery due to these two factors.
When Should I be Concerned About Clicking in Knee?
Infrequent clicking in the knee that is not associated with other symptoms typically does not warrant concern or further evaluation. Clicking in the knee that is increasing in frequency and associated with any of the following symptoms warrants further evaluation.
- Pain
- Swelling
- Locking episodes
- Limited range of motion
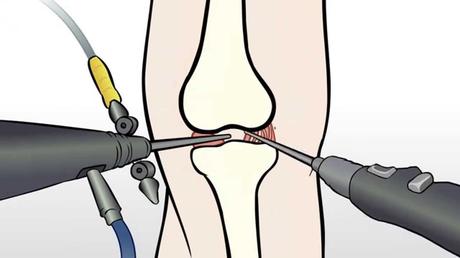
Who should evaluate the clicking in your knee? Bypass your surgeon and schedule a consultation with a physician trained in interventional orthopedics. Surgeons provide surgical solutions that are not always in your best interest. What is interventional orthopedics? It is a board-certified physician in PM& R or anesthesia with advanced orthopedic training with nonsurgical treatment options. They use orthobiologics to heal injured orthopedic tissue. Orthobioligcs are biological substances naturally found in the body that are used to promote quicker healing of muscle, tendon, and bone injuries. To learn more please click on the video below.
How Do I Get my Knee to Stop Clicking?
Identifying the underlying cause of the clicking in the knee will provide the best clinical results. Conservative therapy when appropriate is always the first line of treatment.
Ligament Injuries
Ligament injuries, also known as sprains are common in patients with active lifestyles. There are three grades of sprains.
- Grade 1: ligament is stretched but intact
- Grade 2: partial tear of the ligament
- Grade 3: complete tear
Grade 3 injuries require surgery. Steroids are to be avoided as they are toxic to ligaments and can potentially cause additional damage (6). Treatment options include PRP and a patient’s own bone marrow-derived stem cells. The Centeno-Schultz Clinic are experts in the treatment of ligament injuries. We pioneered the use of bone marrow stem cells in the nonsurgical treatment of ACL tears allowing patients to forgo the risks and complications of traditional ACL graft surgery. The risks of the ACL graft surgery are significant and include a 6x risk of re-tear within 24 months post-surgery (7) and development of arthritis (8).
Meniscus tear
Not all meniscus tears are painful. In fact, in one study 60% of patients without pain had meniscus tears on MRI. PRP is effective in the treatment of meniscus tears. Steroids should be avoided as they are toxic. Meniscus surgery has been demonstrated to be no better than PT (9). In addition it increases the risk of knee instability and arthritis. To learn more about the treatment of meniscus tears please click on the video below.
Osteoarthritis
Knee osteoarthritis is common but does not need to keep you on the sidelines. Mild arthritis can be treated with PRP whereas more advanced cases requires bone marrow stem cells. Knee replacement is major surgery with significant risks and complications. Risks include the need for a second surgery in 6% of patients (10) and patients who undergo knee are 9 times more likely to have a heart attack (11).
Patellofemoral Syndrome
Treatment of patellofemoral syndrome starts with physical therapy. The focus is on improving the tracking of the patella through select muscle strengthening. Loose or damaged knee ligaments can be treated with ultrasound-guided injections of PRP. Often times patients with patellofemoral syndrome also have a lumbar disc and nerve injury that aggravates their knee condition.
In Conclusion
Clicking in the knee can be frustrating. The 5 major causes of clicking are ligament injuries, meniscus tears, knee osteoarthritis, patellofemoral syndrome, and soft tissue. If infrequent and not associated with other symptoms typically does not warrant further evaluation. If clicking in the knee is increasing in frequency and associated with pain, swelling, locking episodes, and limited range of motion evaluation is indicated. The clicking is a warning sign that you have a problem that needs attention. Surgeons provide surgical solutions. A physician trained in Interventional Orthopedics can provide you with a range of nonsurgical treatment options. Treatment for clicking in the knee requires the underlying cause to be identified. The Centeno-Schultz Clinic Physicians are experts in the treatment of clicking in the knee. Treatment options include PRP and stem cell injections.
If the clicking in the knee is increasing and associated with pain, swelling or limited range of motion this is a warning sign. Act now before the problem gets bigger and the options are limited. Schedule a Telemedicine consult with a board-certified physician who can review your history, studies, and provide you the best nonsurgical treatment option. Listen to your body as it is warning you!
1.Hastings DE. Diagnosis and management of acute knee ligament injuries. Can Fam Physician. 1990;36:1169-1189.
2. Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM. Treatment of meniscal tears: An evidence based approach. World J Orthop. 2014;5(3):233-241. Published 2014 Jul 18. doi:10.5312/wjo.v5.i3.233.
3. Snoeker BAM, Bakker EWP, Kegel CAT, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther 2013;43:352-367.
4. Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med. 2011;2(2):205-212.
5. Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T. Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol. 2011;38(5):921-930. doi:10.3899/jrheum.100569.
6. Wernecke C, Braun HJ, Dragoo JL. The Effect of Intra-articular Corticosteroids on Articular Cartilage: A Systematic Review. Orthop J Sports Med. 2015;3(5):2325967115581163. Published 2015 Apr 27. doi:10.1177/2325967115581163
7. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567-73.doi: 10.1177/0363546514530088.
8.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049-57. DOI: 10.1177/0363546514526139.
9.Collins JE, Losina E, Marx RG, et al. Early Magnetic Resonance Imaging-Based Changes in Patients With Meniscal Tear and Osteoarthritis: Eighteen-Month Data From a Randomized Controlled Trial of Arthroscopic Partial Meniscectomy Versus Physical Therapy. Arthritis Care Res (Hoboken). 2020;72(5):630-640. doi:10.1002/acr.23891
10. Pabinger C, Berghold A, Boehler N, Labek G. Revision rates after knee replacement. Cumulative results from worldwide clinical studies versus joint registers. Osteoarthritis Cartilage. 2013 Feb;21(2):263-8. doi: 10.1016/j.joca.2012.11.014.
11. Lu N, Misra D, Neogi T, Choi HK, Zhang Y. Total joint arthroplasty and the risk of myocardial infarction: a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015;67(10):2771–2779. doi: 10.1002/art.39246

