The neck pain is always there. It started as a gradual ache and now has progressed. Your doctor ordered tests. What is cervicalgia? What are the causes of cervicalgia? What are the symptoms associated with cervicalgia? How is cervicalgia diagnosed? What are the treatment options for cervicalgia? Let’s dig in.
What Is Cervicalgia? AKA Neck Pain
Cervicalgia is a broad, non-specific term to describe neck pain. It is common and affects approximately 2/3rd of the population at some point in their lives. It is the fourth major cause of disability (1). Various epidemiological studies have reported prevalence from 15-50% (2). Risk factors for neck pain include prior history of musculoskeletal pain, high quantitative jobs, low social support, job insecurity, low physical strength, and poor computer station design (3).
What Are the Causes of Cervicalgia?
There are many different causes of neck pain. The most common cause of cervicalgia include
Muscle Injury
Injury to the muscle is also known as strain and typically is the result of overactivity or trauma. It typically improves with conservative care.
Facet Injury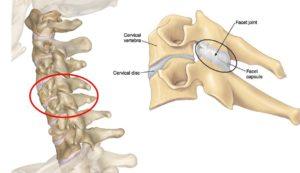
A facet is a small joint on the backside of the spine that provides stability and limits rotation. It is susceptible to injury. Pain arising from the facet joint has been well studied. Each joint has a distinct referral pattern which is illustrated to the right. For example injury to the C5/6 facet joint typically results in pain in the shoulder and wing blade area. Injury to the facet joint can cause cervicalgia.
Disc Injury
The disc is an important shock absorber sandwiched between the boney building blocks of the spine. Discs are susceptible to injury. Common disc injuries include disc protrusion, disc bulges, and disc herniations all of which can cause cervicalgia.
Spinal Nerve Injury/ Compression
At each level of the spine, a spinal nerve exits the spinal column through a boney doorway. The doorway is called the neural foramen. The exiting nerve can be irritated or compressed by disc protrusions, facet overgrowth, thickened ligaments, and bone spurs. Common symptoms include electrical radiating pain down one or both arms which can extend into the fingers. Numbness and tingling may occur. Spinal nerve irritation is a frequent cause of cervicalgia.
Ligament Injury
Ligaments are thick pieces of connective tissue that connect one bone to another. They provide important stability for the cervical spine. Damage or injury of the ligament can result in excessive movement of the structures in the spine. This is called instability and can cause additional wear and tear on the discs, facets, and nerves. Ligament injury can cause cervicalgia
Poor Posture

The neck is a series of boney building blocks that stack upon one another. Neutral spinal alignment is essential for the proper function of the muscles, joints, and discs. Regrettably, computer screens, tablets, and cell phones have compromised this spinal alignment placing excessive demand on the supporting muscles, ligaments, and tendons. Over time the facet joints and discs become irritated and injured. Neck pain soon develops. Poor posture is a significant cause of cervicalgia in 2020.
Stress and Psychological Issues
Stress and psychological issues are causes muscle tension in the neck. If persistent, this can change the alignment of the spine with resultant pain and limitation.
Symptoms
Symptoms vary depending upon the underlying source of neck pain and the severity of the injury. Common symptoms include:
- Neck Pain
- Muscle Tightness or Spasm
- Difficulty in Moving Your Head
- Headaches
- Shoulder Pain
- Thoracic Pain
- Pain in the arm, forearm, or hand.
- Electrical Shooting Pain from the Neck into Fingers
- Numbness in the Hand and Fingers
- Weakness in the Arm, Hand, or Fingers
How to Diagnose Cervicalgia
The diagnosis of cervicalgia starts by taking a detailed history from the patient. Important questions include:
- The onset of symptoms: Were they abrupt or gradual?
- History of trauma
- History of infections
- What aggravates the pain?
- What alleviates the pain?
- Quality of pain: Is it dull or sharp in character?
- The severity of the pain: Is it mild or severe?
- Treatments to date and their effectiveness.
A thorough physical examination is required. Muscle strength, range of motion, and reflexes, must be evaluated along with a full neurologic examination. The imaging study of choice is MRI as it examines muscles, ligaments, tendons, nerves, cartilage, and bone. X-ray is not appropriate as it only evaluates boney structures. Laboratory tests are often required to evaluate for the presence of infectious or metabolic conditions. If questions still remain additional studies may be performed including electrodiagnostic studies such as an EMG (Electromyography) .
How to Treat Cervicalgia
Treatment is dependent upon the underlying condition. Conservative care is the first-line treatment when appropriate. This may include:
Conservative
- Rest
- Heat or ice compresses
- Safe anti-inflammatory medications such as fish oil and Turmeric
- Stretching
- Good posture with neutral spine alignment: Say goodbye to the rounded shoulders and collapsed chest.
- Chiropractic care
- Physical therapy
Steroids
When conservative therapy fails to provide relief many patients are referred for steroid injections. Steroids are powerful anti-inflammatory agents that should be avoided as they are toxic to cartilage and other orthopedic tissue and have significant side effects including bone death and osteoporosis (4).
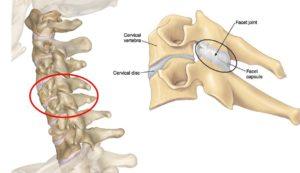
Surgery
Surgery is oftentimes recommended for patients with disc and spinal nerve injuries that do not respond to conservative therapy. There are a number of different surgeries for these conditions. A common surgical solution is a cervical fusion. This is a major surgery where a disc is removed and replaced with bone or a spacer and the spinal bones are stabilized by screws and plates. Fusion is no guarantee that the pain will improve. There are significant complications associated with fusion which include:
Infection
Failure: The bones do not fuse
Nerve injury
Adjacent Segment Disease: This is a condition where there is additional pressure placed on the disc and facets above and below the level of the fusion. This added pressure leads to degeneration, pain, and often times the need for additional surgery.
To learn more about adjacent segment disease please click on the video below.
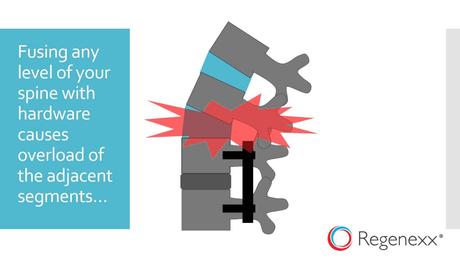
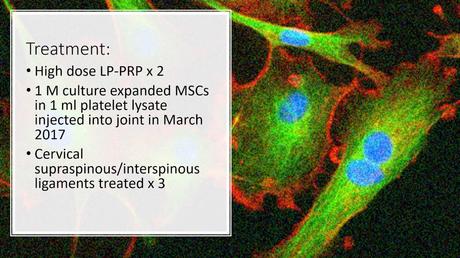
Regenerative Options
At the Centeno-Schultz Clinic, we are experts in the diagnosis and treatment of neck pain. We have 15 years of experience treating disc, facet, ligament, spinal nerve, and ligament injuries. Treatment options include PRP and a patient’s own stem cells. In 2005 we were the first clinic in the world to inject stem cells into the disc. PRP is rich in growth factors that can increase blood flow, decrease inflammation, and accelerate healing. Stem cells are powerhouses of regeneration and repair using different pathways throughout the body to promote healing.
To learn more about the destructive consequences of repeated steroid injections and how stem cells healed a severe cervical facet injury please click on the video below.
In Conclusion
Cervicalgia is a broad, non-specific term to describe neck pain. It is common and affects appropriately 2/3rd of the population at some time in their lives. There are multiple causes of cervicalgia. The most common include injury to muscles, discs, facets, spinal nerves, and ligaments in the neck. Other sources of neck pain include poor posture, stress, and psychological issues. Symptoms vary and may include neck pain, muscle tightness, difficulty moving your head, headaches, shoulder pain, thoracic pain, arm weakness, and numbness and tingling. Diagnosis starts with a history and physical examination. MRI is the study of choice. Laboratory tests and additional tests such as EMG can also be used. Conservative care when appropriate is the first-line treatment of choice. Steroids should be avoided as they cause damage to tendons, ligaments, and cartilage. Surgery is associated with significant risks including failure, infection, and adjacent segment disease. PRP and a patient’s own stem cells are effective, natural treatment options.
Neck pain is a progressive condition that can get worse over time if you don’t take action. Taking pills and hoping that it will go away is not effective. Dependence on medication has significant risks which include increasing your risk for heart attack, GI bleed, dependence, and addiction. Schedule a Telemedicine consultation with a board-certified, fellowship-trained physician and learn about your regenerative treatment options. Act now while the issue is small and treatment is available. Get your life and level of activity back today!
1.Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, Dellavalle R, Danaei G, Ezzati M, Fahimi A, Flaxman D, Foreman, Gabriel S, Gakidou E, Kassebaum N, Khatibzadeh S, Lim S, Lipshultz SE, London S, Lopez, MacIntyre MF, Mokdad AH, Moran A, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Pope C, Roberts T, Salomon J, Schwebel DC, Shahraz S, Sleet DA, Murray, Abraham J, Ali MK, Atkinson C, Bartels DH, Bhalla K, Birbeck G, Burstein R, Chen H, Criqui MH, Dahodwala, Jarlais, Ding EL, Dorsey ER, Ebel BE, Ezzati M, Fahami, Flaxman S, Flaxman AD, Gonzalez-Medina D, Grant B, Hagan H, Hoffman H, Kassebaum N, Khatibzadeh S, Leasher JL, Lin J, Lipshultz SE, Lozano R, Lu Y, Mallinger L, McDermott MM, Micha R, Miller TR, Mokdad AA, Mokdad AH, Mozaffarian D, Naghavi M, Narayan KM, Omer SB, Pelizzari PM, Phillips D, Ranganathan D, Rivara FP, Roberts T, Sampson U, Sanman E, Sapkota A, Schwebel DC, Sharaz S, Shivakoti R, Singh GM, Singh D, Tavakkoli M, Towbin JA, Wilkinson JD, Zabetian A, Murray, Abraham J, Ali MK, Alvardo M, Atkinson C, Baddour LM, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dellavalle RP, Jarlais, Dicker D, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Foreman, Forouzanfar MH, Freedman G, Freeman MK, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayarman S, Johns N, Kassebaum N, Khatibzadeh S, Lan Q, Leasher JL, Lim S, Lipshultz SE, London S, Lopez, Lozano R, Lu Y, Mallinger L, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran A, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Raju M, Razavi H, Ritz B, Roberts T, Sacco RL, Salomon J, Sampson U, Schwebel DC, Shahraz S, Shibuya K, Silberberg D, Singh JA, Steenland K, Taylor JA, Thurston GD, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wulf S, Murray; U.S. Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013 Aug 14;310(6):591-608. doi: 10.1001/jama.2013.13805. PMID: 23842577; PMCID: PMC5436627.
2. Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006 Jun;15(6):834-48. doi: 10.1007/s00586-004-0864-4. Epub 2005 Jul 6. PMID: 15999284; PMCID: PMC3489448.
3.Kanchanomai S, Janwantanakul P, Pensri P, Jiamjarasrangsi W. Risk factors for the onset and persistence of neck pain in undergraduate students: 1-year prospective cohort study. BMC Public Health. 2011;11:566. Published 2011 Jul 15. doi:10.1186/1471-2458-11-566
4.Wernecke C, Braun HJ, Dragoo JL. The Effect of Intra-articular Corticosteroids on Articular Cartilage: A Systematic Review. Orthop J Sports Med. 2015;3(5):2325967115581163. Published 2015 Apr 27. doi:10.1177/2325967115581163

