Dr. Jason Markle discusses Baxter’s Neuropathy, its symptoms, causes, and potential treatments.
Transcript
Good afternoon, Dr. Markle of Centeno-Schultz Clinic, and today we’re discussing a condition called Baxter’s Neuropathy. It’s one of the many things that can create some chronic and intense heel pain. So we’ll be discussing
- what exactly causes Baxter’s neuropathy,
- some symptoms, as well as
- some underlying issues that can create it.
And, in addition, discussing some Regenerative Medicine and non-surgical interventional techniques for successful treatment of Baxter’s Neuropathy.
What is Baxter’s Neuropathy?
It is an entrapment syndrome, like carpal tunnel syndrome in your hand. This is an entrapment of a nerve in your foot, right around your heel, on the inside part compressing a branch of your tibial nerve called your inferior calcaneal nerve, and that is the Baxter’s nerve. Now, the inferior calcaneal nerve is the first branch of the lateral plantar nerve, which is a branch off your tibial nerve. It lives between a muscle belly called your abductor hallucis muscle, as well as the medial calcaneal tuberosity, which is a small bump where a common heel spur occurs in the foot.
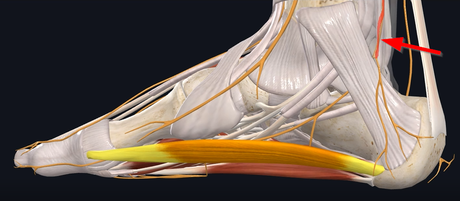
Now, if we look at the way the nerve travels – So the tibial nerve comes down (see Figure 1).
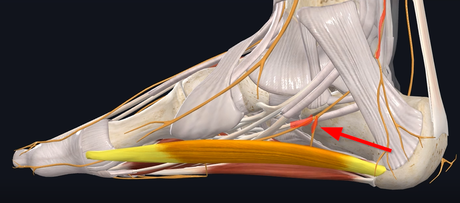
and then branches into your medial and lateral plantar nerve and then the nerve branches again into that Baxter’s nerve (see Figure 2).
It goes by this muscle right here, which is to your abductor hallucis muscle. And then, after it gets past that muscle, it goes adjacent to your calcaneal tuberosity and your quadratus plantae muscle, which is at the base of the foot right there, and here’s the nerve going right under it, and then it traverses (see Figure 3).
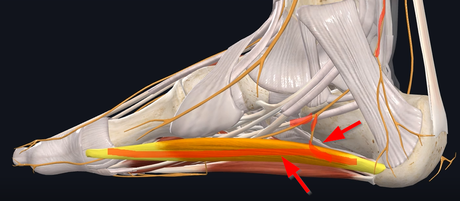
posteriorly around. Sometimes, there are common heel spurs in this area. Those three areas are the main regions and potential entrapments that create the entrapment itself.
Causes of Baxter’s Neuropathy
Now causes of Baxter’s Neuropathy – sometimes you have some predisposing conditions, one such as muscle hypertrophy, meaning if one of those two muscles in the foot become overworked and hypertrophied, they can compress the nerves traveling around it. Obesity can be problematic. Then foot and ankle conditions such as hyper-pronation or flat feet can create some compression of that nerve.
If you have some bone spurs that were created from plantar fasciitis, or just irritation around the nerves, that can also create some bony compression of that nerve.
Symptoms
Now Symptoms. A common – if we are looking at heel pain in general – diagnosis has always been plantar fasciitis. Now plantar fasciitis, typically, historically, has been pain first thing in the morning; you have pain directly into the heel bone. That first step or two in the morning becomes excruciating, and it loosens up as you stretch out the tissue.
Now, Baxter’s neuropathy is the exact opposite – meaning: you really don’t have any pain in the morning, but towards the end of the day. Meaning: you’re walking on a nerve that’s getting irritated. So, the more you walk on it, the more that nerve gets irritated. So, pain tends to be at the end of the day. Irritation of that nerve can create some paresthesia, meaning numbness and tingling, along the bottom part of the heel.
As well as from an examination, if you can palpate the course of where the nerve is, you can elicit and aggravate the patient’s pain and replicate it.
Now, if you have these symptoms, how do you prove its back neuropathy?
You can get an x-ray that can show the pathology of a potential bone spur in that area. MRI can show if the muscles have hypertrophied around it, causing some compression of that nerve, as well as compression of the nerve does create some fluid and inflammation around that nerve and some thickening of the fascia itself.
How Do You Treat Baxter’s Neuropathy?
One of the common ways would be medications. So typically your primary care physician or physician starts you off on some sort of anti-inflammatory, or if you describe some burning neuropathic pain symptoms, they’ll put you on a neuropathic pain medication such as Gabapentin, Lyrica or a host of any other neuropathic medications. If you have any underlying issues, such as the flat fee or hyper-pronation, there are foot and ankle braces. They can help to help take some pressure off the nerve.
If all those fail, then injection-based treatments would be corticosteroid injections, where if there’s any inflammation around the nerve, those steroids help shut down that inflammation. But the problem with this long term is it actually is toxic to the nerve cells. So, it could potentially make those symptoms worse, long term-wise, which, when it does come back, it could create damage to the muscles or tendons around it also re-aggravating that area. Opposite to that would be a surgical treatment, which is surgical decompression.
Now, here at Centeno-Schultz Clinic, we pride ourselves as some of the founders of the field of Regenerative Medicine, and, utilizing regenerative medicine such as platelet rich plasma in the form of platelet lysate, we’ve been able to utilize this in treating nerve pain for many years. We have published multiple papers, such as sciatica using PRP epidurals in the extremities. A lot of times we use musculoskeletal ultrasound to hydrodissect the nerve with the platelets. And that accomplishes two things at once.
- We’re creating some space around the nerve that was getting entrapped.
- We’re putting growth factors around the nerve to help those nerves repair.
And if one of the issues is a potential bone spur, then we can also utilize a technique called a Tenex Osteotomy, where we take a small device, under ultrasound guidance, and actually break up the bone spur and remove the bone spur subcutaneously, or percutaneously – meaning through the skin just with a simple needle.
If we look at this video, we can see the nerve in the elbow right here:
And here is the bone spur. And we can see the machine, under ultrasound guidance, breaking up the bone spur. This gentleman was having intense pain in the elbow, as well as numbness and tingling. Within probably a week or two, he was nearly asymptomatic, and the pain has not come back since doing this procedure. Again, this was a combined Tenex procedure to remove the bone spur and then utilizing the PRP as an injectate to hydrodissect the nerve around it and give that nerve some space around it.
So, if you have been dealing with any heel pain issues and numbness and tingling and potentially been diagnosed with Baxter’s neuropathy, give us a call. We are happy to evaluate you either via telemedicine or in-person evaluation and discuss potential treatment options and further evaluate you to see some of the small details of exactly what is causing some of your symptoms.
Thank you and have a good day.

