
 Happy Pumpkin Day folks, and to celebrate this day of weird encounters, I am going to reel off a list of the commonest peeves I have experienced in the past couple of years I have been doing Medicine. There are obvious gaps in the stories, and many are not even unique to me, but I must say, the more you read stuff and go “Its so totally happened to me”, the worse off we are. Now let me make it very clear right at the outset that I am not apportioning any blame on either parties (heck, both doctors AND patients are at fault!) but just stating some things as they are.
Happy Pumpkin Day folks, and to celebrate this day of weird encounters, I am going to reel off a list of the commonest peeves I have experienced in the past couple of years I have been doing Medicine. There are obvious gaps in the stories, and many are not even unique to me, but I must say, the more you read stuff and go “Its so totally happened to me”, the worse off we are. Now let me make it very clear right at the outset that I am not apportioning any blame on either parties (heck, both doctors AND patients are at fault!) but just stating some things as they are.
I will try to take a look into some common poor patient behaviors we, as doctors, either actively or passively, encourage in our daily clinical encounters, putting them down to the fact that it is not harming anyone.
1. Antibiotics for the Sore ThroatThis has to be one of the commonest peeves of mine and any other doctor dealing with patients on a day to day basis. I have recently had an ugly encounter with a patient with a similar problem. A few weeks ago, a viral infection was doing the rounds in my locality, which started off with a sore throat, worsened over the next few days, led to 5-10 days of fever with myalgia and prostration and resolved without any apparent complications with supportive treatment (as is the wont with most viral infections).
So I had a middle aged male who walked in with a day of symptoms suggestive of this condition and I decided to treat him with Paracetamol/Ibuprofen, oral fluids and rest. However, he was VERY insistent that he needed an antibiotic to get well, and to placate his fears and establish the absence of any bacterial infection, I sent off a battery of (unnecessary, expensive) investigations. They all came back within normal limits on the 3rd day of his illness. Meanwhile, he was hitting the worst part of his viral infection (note that he was not following any of the medications or rest I had advised for him), and was getting really cranky. When I finally told him that his viral sore throat would not be ameliorated with a dose of antibiotics, he got furious, called me a quack, and left.
A doctor next door obliged him with a script for Cefixime, to be taken for 10 days (it was already his 3rd day of the disease, remember). He got well soon enough, thanked the antibiotic happy doc profusely, swore some more at me, and left.
While obviously I am bitter about this issue, the easy way out (and also to gain a paying patient) is to give it to him and be done with it. The other doctor is more experienced than me, and I am sure he too realized that what he was doing with the antibiotic script was basically buying time while the disease ran its course. However, he caved in to the demands of the patient. While I believe I tried my best to counsel the patient and tell him the futility of the antibiotic script, now he believes that those drugs cured him of his miserable illness, so the next time he gets a sore throat he will go more ballistic demanding antibiotics.
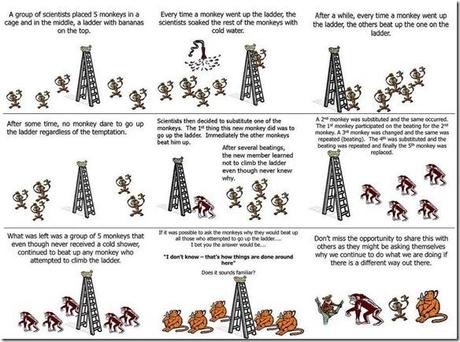
Not only are we not preventing the poor, antibiotic demanding behavior of patients, we are also, by default, reinforcing the habit in them… But of course, I am not asking you to trust what I am saying. This is the age of information, and everything is available at the click of a mouse. Check out this Cochrane Review (1) written by Paul Glasziou et al, which finally concludes, in a modest manner:
Antibiotics confer relative benefits in the treatment of sore throat. However, the absolute benefits are modest. Protecting sore throat sufferers against suppurative and non-suppurative complications in modern Western society can only be achieved by treating many with antibiotics, most of whom will derive no benefit. In emerging economies (where rates of acute rheumatic fever are high, for example), the number needed to treat may be much lower for antibiotics to be considered effective. Antibiotics shorten the duration of symptoms by about sixteen hours overall.
Really? Is it worth the cost and risk of side effects? Especially when India is all set to emerge as the antibiotic resistance capital of the world?
2. Free drugs are bad drugsThis is a problem which has two sides. One seen in the government hospital, and one in private practice. Here I will talk about the latter.
I spent all of my years working and training in a government hospital, where the patients are mostly so poor that they can barely afford  three square meals a day, let alone the expensive medicines that they need for their medical conditions. So, in order to dispense the best possible care that they would adhere to, it has become a bit of a second nature to prescribe drugs that are a little cheaper (sometimes writing the generic name instead of the trade/brand names helps). Now I do not mean that I do not prescribe the recommended drugs for a certain condition just based on cost considerations. Most certainly, I do. But I try to write a drug which is a little cheaper, out of patent, available as a generic, etc. so tat the patient can buy the recommended drug for the lowest possible price. But now that I am seeing some patients that do not fall into the same bracket, I am faced with a unique problem!
three square meals a day, let alone the expensive medicines that they need for their medical conditions. So, in order to dispense the best possible care that they would adhere to, it has become a bit of a second nature to prescribe drugs that are a little cheaper (sometimes writing the generic name instead of the trade/brand names helps). Now I do not mean that I do not prescribe the recommended drugs for a certain condition just based on cost considerations. Most certainly, I do. But I try to write a drug which is a little cheaper, out of patent, available as a generic, etc. so tat the patient can buy the recommended drug for the lowest possible price. But now that I am seeing some patients that do not fall into the same bracket, I am faced with a unique problem!
When a person came in complaining of an allergic rhinitis (they had a problem with smoke and dust and this is the festival season, and people are cleaning their homes and burning crackers all day long, so put two and two together!), I prescribed a generic antihistaminic (very cheap) which is supposedly very effective for this condition and asked the patient to stay away from the allergenic stimuli. They came to me a couple of days later complaining that they were not better, and needed some other drugs. On enquiry, the patient admitted to cleaning the home in the afternoons and lighting crackers in the evening both the preceding days!
Now I reiterated my old advice and sent her off.
Later on, I learnt that the patient had gone to another doctor, who had prescribed a laundry list of super expensive drugs, comprising of the SAME antihistaminics (of a fancier brand), some vitamin capsules and, hold your breath, Coamoxiclav (Amoxicillin + Clavulanate, an antibiotic given to patients with beta lactamase producing bugs). And the patient was seen happily lighting crackers all night long!
A similar experience was related to my by a colleague who was a little shocked to note that people who avoided the free immunization clinics under the National Immunization Schedule run in the government hospitals were not averse to vaccinating their children. They, in fact, went to the private practitioners for the SAME vaccinations and paid thousands of rupees for EACH dose. The reason? They thought that since the hospitals were giving away the vaccines for free they were of a poorer nature!
And if you do not trust my words, read up Dan Ariely’s workk in JAMA (2). He gave 2 groups of volunteers the same placebo, told one group its an analgesic that costs 2.5$ and the other 10 pence. And guess which group felt better pain relief when they took the meds? Of course, for two and a half pop a tablet, you are bound to feel all that more comfortable, aren’t you?
3. Pour Some Saline IN Me!This issue is more frequently encountered in the ER of a government hospital.
This is the unique medical therapy in which all kinds of diseases are cured by the magic potion of IV Normal Saline infusion. One other magic drug that ALL patients who came to my ER expected was a nasal prong attached to an oxygen cylinder (which was often empty, since these patients did not need it anyways).
I did not realize the roots of this issue until I went to serve out my rural posting out in the middle of nowhere. Most patients that came through the doors of that dilapidated place were either handled by quacks or ojhas before they came, so by the time they came in, they were pretty out of it and the only thing the attending physician could do was to gain an IV access, start an IV Saline drip and refer him off to a state hospital which could take care of these complicated cases. Now, surprisingly, more often than not, the very maneuver of pushing in an iv cannula and running some fluids would raise the patient from the dead!
Apparently this is the situation out there in many of the primary health care centers which do not have too many other drugs to dispense anyways.
Besides, I have noted an unshakeable belief that paani chadhaana (pouring the water, literally) is the best of all medicines possible. In fact, I kid you not, once I had this guy walk through the ER telling us that he felt very tired all the time and needed some IV Saline to get up and about (he was VERY anemic, if you still care, by the way).
Often, when the ER is overflowing with trauma patients needing resuscitating and myocardial infarcts needing thrombolysis and blocked up guts needing to be prepped for emergency surgery, we have these more benign cases that we can keep waiting for some time. But more often than not, to give the impression of doing something, we push in the IV cannula and start a drip to keep it patent, or put on the nasal prongs just to make them a little comfortable while they wait (does that even work?). And often, by the time the storm has blown over, the symptom with which these people walked in with are gone and they go home praising the hyperactive doctor, the Oxygen and of course, paani!

In one of the most innovative, yet startling papers published in the New England Journal of Medicine (3), the ugly truth behind the need for knee surgery (arthroscopic lavage or arthroscopic debridement) in osteoarthritis has been unveiled. The study had created a lot of waves when it came out, but in conclusion, the authors unambiguously note, and I quote:
In this controlled trial involving patients with osteoarthritis of the knee, the outcomes after arthroscopic lavage or arthroscopic débridement were no better than those after a placebo procedure.
How much more damning does it get?
The study, by the way, was a placebo controlled trial of surgery. The group getting the sham surgery were put under light anesthesia and were not aware of their operative status. Oh, and take a look at the beautiful manner in which the placebo patients were dealt with:
Placebo Procedure:To preserve blinding in the event that patients in the placebo group did not have total amnesia, a standard arthroscopic débridement procedure was simulated. After the knee was prepped and draped, three 1-cm incisions were made in the skin. The surgeon asked for all instruments and manipulated the knee as if arthroscopy were being performed. Saline was splashed to simulate the sounds of lavage. No instrument entered the portals for arthroscopy. The patient was kept in the operating room for the amount of time required for a débridement. Patients spent the night after the procedure in the hospital and were cared for by nurses who were unaware of the treatment-group assignment.
Postoperatively, there were two minor complications and no deaths. Incisional erythema developed in one patient, who was given antibiotics. In a second patient, calf swelling developed in the leg that had undergone surgery; venography was negative for thrombosis. In no case did a complication necessitate the breaking of the randomization code.
Who says there is no elegance in surgical research?
In conclusion: When in doubt, follow “The 13th Law”!The 13th Law of the House of God is:
THE DELIVERY OF GOOD MEDICAL CARE IS TO DO AS MUCH NOTHING AS POSSIBLE.What? Never heard of the House of God, Samuel Shem’s masterful classic on the shenanigans of the medical profession? Go get one right now!
Anyways, as I was saying, I completely agree with what Lisa Rosenbaum states in her opinion piece in the NEJM (4):
When my grandfather practiced, the physician, in the cultural imagination, was paternalistic, even stern. But this image was accompanied by an implicit trust in physicians’ dedication to patients’ well-being. In the absence of all the tools that now forge the bond between patient and physician, words mattered far more. So did touch. A pat on the back and some simple reassurance could satisfy expectations, even make people feel better.
Can we reconsider what it means to “do nothing”? The value of this concept remains ours to determine.
“Patients don’t expect me to perform miracles,” he concludes. “They leave that up to the priest. All they ask of me is that I do my best and offer them sympathy when I fail. If I had realized this before, I would have gone to many more funerals.”
The fat man (HoG reference) was completely correct when he stated the need to do as much nothing for your patients as possible. Maybe sometimes as doctors, we realize deep down inside that there is little we can do to alleviate the suffering of the fellow human being in front of us and hence indulge in doing something, anything, in the hope that it helps the ailing person, and in the hope that it helps blunt our sense of helplessness. However, sometimes, in doing this, we do more harm than good. Today, modern medicine has progressed at the rate of knots and we stand at the crossroads where we are toying with the principles of life itself. The entire human genome lies at our feet, we can use biological agents to modify physiological responses, there is not one nook or cranny inside the human body that we cannot look into.
Medicine has given us a lot of tools, but still, we are unable to cure the common cold.
The irony is, years ago, Voltaire had hit the nail hard on the head when he said:
The purpose of medicine is to amuse the patient until nature effects a cure.
The problem is, in amusing the patient, we end up reinforcing behaviors that make the delivery of the best possible healthcare a bit of a pain. The truth is in today’s world, the patient is the king. We, as doctors, no longer cater to patients, but to healthcare consumers. And as service providers, much of the stress goes on to the nebulosu issue of consumer satisfaction. My patient bad mouthed me to the community though I stuck to the proper clinical protocols. While I may be naïve enough to not be swayed by this and stand my ground, most would consider the easier (and financially safer) way out and give in to the (unreasonable) demands of the patients. Also, on the other hand, we as physicians, often use these follies of the patients in order to effect our cures. We give the attention seeker a false jab, we load the aches/pains with an IV drip, we give multivitamins to the frequent flying hypochondriacs… and they work!
A similar issue has been highlighted in yesterday’s New York Times by Tara Parker-Pope, albeit in a bit of a different light.
Where does the solution lie? A blanket answer is difficult to formulate and much depends on the particular issue at hand. For example, the next time I get the fever guy (if at all) with an0ther bout of viral fever, I would ask him to keep a fever chart for a couple of days, give him some safe home remedies, maybe some vitamins, because clearly, he needs the drugs to feel as if something is happening… in short, keep him occupied and amused while nature affects her cure.
The answer is not in tricking. It lies in treating… Happy Halloween everyone!
1. Del Mar CB, Glasziou PP, Spinks AB. Antibiotics for sore throat. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD000023. Review. PubMed PMID: 17054126.
2. Waber RL, Shiv B, Carmon Z, Ariely D. Commercial features of placebo and therapeutic efficacy. JAMA 2008;299:1016-7
 3. Moseley, J., O’Malley, K., Petersen, N., Menke, T., Brody, B., Kuykendall, D., Hollingsworth, J., Ashton, C., & Wray, N. (2002). A Controlled Trial of Arthroscopic Surgery for Osteoarthritis of the Knee New England Journal of Medicine, 347 (2), 81-88 DOI: 10.1056/NEJMoa013259
3. Moseley, J., O’Malley, K., Petersen, N., Menke, T., Brody, B., Kuykendall, D., Hollingsworth, J., Ashton, C., & Wray, N. (2002). A Controlled Trial of Arthroscopic Surgery for Osteoarthritis of the Knee New England Journal of Medicine, 347 (2), 81-88 DOI: 10.1056/NEJMoa013259
4. Rosenbaum L. The art of doing nothing. N Engl J Med. 2011 Sep 1;365(9):782-5. PubMed PMID: 21879895.
