[An examination of Pauling’s research on vitamin C and heart disease, part 3 of 4.]
In early 1991, Dr. Howard Bachrach of Southold, New York informed Linus Pauling of experimental results indicating that lipoprotein (a) [commonly abbreviated as Lp(a)] binding to arterial walls could be suppressed through the use of supplemental lysine. In the weeks that followed, Bachrach continued to exchange information with Pauling and his colleague at the Linus Pauling Institute of Medicine, Matthias Rath, in hopes of determining if lysine, vitamin C, or some combination of the two might not only prohibit but actually reverse plaque accretion in vitamin C-deficient guinea pigs.
A breakthrough came about on February 28, 1991 – Linus Pauling’s 90th birthday – when Rath reported to his colleagues his finding that Lp(a), as synthesized in the liver, was in fact regulated in an unknown way by the amount of vitamin C present in the body.
Lp(a) was understood by Rath and Pauling to form from low density lipoprotein (LDL) and Apoliprotein A-1 [abbrevied apo(a)] in the liver in amounts largely determined by the rate of synthesis of apo(a). This rate of synthesis was increased by low vitamin C concentrations in the blood. Rath and Pauling published the finding in Medical Science Research, arguing that plaque formation was not caused by LDL cholesterol, as previously thought, but lipoprotein (a) instead. Crucially, high doses of vitamin C was identified by the authors as being central to reducing these dangerous lipoprotein (a) levels.
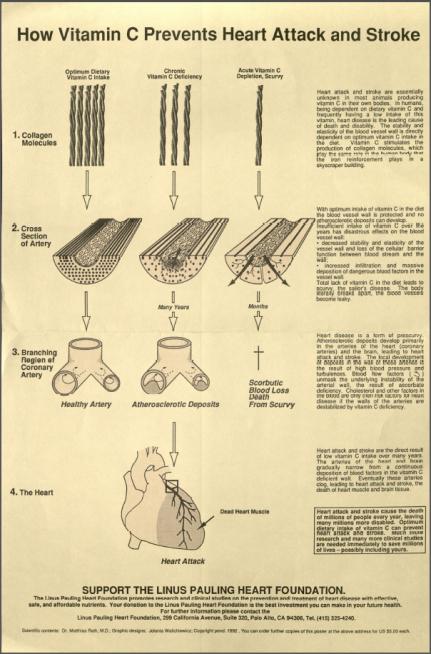
This discovery formed the basis for what Pauling and Rath would eventually call their Unified Theory of Human Cardiovascular Disease. Fundamental to this framework was Pauling and Rath’s belief that cardiovascular disease was a degenerative disease caused by vitamin C deficiency. The theory also put forth that humans’ inability to synthesize their own vitamin C drove the disease, though it was also aggravated by genetic defects and exogenous risk factors, such as free radicals introduced by cigarette smoke or oxidatively modified triglyceride-rich lipoproteins exerting a noxious effect on the vascular wall.
Further, lipoprotein (a) was put forth as an evolutionary surrogate for vitamin C in animals – like primates and guinea pigs – that no longer produced their own ascorbic acid. This collection of species shows much higher levels of Lp(a) in the blood, a characterstic seen by Pauling and Rath as serving as an ad hoc biological mechanism used by the body to repair damaged tissues through deposit on weakening arterial walls. Too much Lp(a), however, leads to plaque formation, causing angina, heart attack, and stroke. A lack of vitamin C thus leads indirectly to the deterioration of arteries.
From there, the researchers argued that this problem could be easily fixed if only the recommended doses of vitamin C were increased to levels many times larger than those prescribed by the federal government. Were the body enabled to make use of supplemental vitamin C to produce collagen – as all animals that synthesize vitamin C internally do – humans would be much more efficient at repairing damaged arterial walls. Indeed, vitamin C could function not only to strengthen arterial walls, but also to reduce the amount of Lp(a) being produced by the body and consequently – as a co-factor in the hydroxylation reaction that converts cholesterol to bile acids – lowering the amount of free cholesterol in the blood as well.
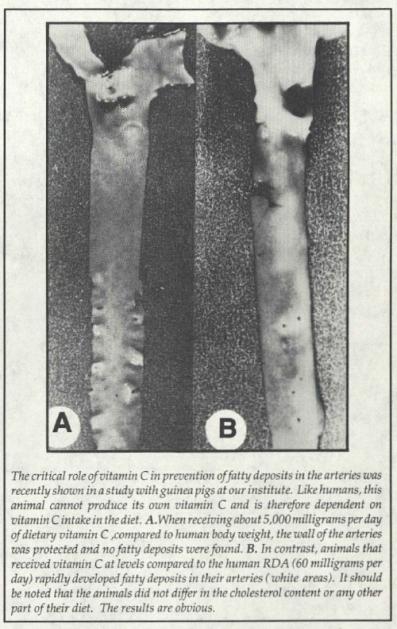
Published in the Linus Pauling Institute of Science and Medicine Newsletter, March 1992.
To Pauling and Rath, the logic supported their theory was clear. Critics, however, demanded large clinical studies to support the claims, and this was research that the Institute, which was struggling mightily for funds, did not have the resources to pursue.
It was at this point that other interested researchers took up the torch. One of them, Dr. James Enstrom at UCLA, led a 1992 study of over 11,000 human subjects. Enstrom’s work indicated that those individuals who regularly took supplements of vitamin C at federally recommended levels enjoyed significantly lower rates of heart disease than did those not subscribing to a supplementation routine. This data led Enstrom’s team to wonder – in tandem with Pauling and Rath – whether larger doses would achieve an even greater protective effect.
In 1993, hoping to add additional support to the hypothesis, Pauling published three case studies in the Journal of Orthomolecular Medicine. Each study focused on individuals who had suffered from severe cardiovascular disease and undergone surgical procedures, including heart bypass. The individuals in question had read Pauling’s papers with Rath and had decided to try adding lysine and vitamin C to their diet. In certain cases, members of the study group had already been taking fairly high doses of vitamin C and then added lysine.
The 1993 data clearly were not anything like controlled studies and were reported on anecdotally by Pauling. Further, the amounts of lysine and vitamin C ingested varied significantly between individuals, but was generally in the range of between 3 to 6 grams per day of each supplement. Many within the study group reported rapid relief and positive responses.
Though far from authoritative, the published case studies did help to bolster Pauling and Rath’s position, attracting increased interest in the work. However, the duo also received plenty of letters, some filled with irritation, from people who had incorporated supplementation and saw no positive change. Some correspondents, in fact, were getting worse.
