We’ve reached the off-season for most northern hemishphere triathletes. Our regular readers here at Endurance Corner will know that our daily articles have begun to focus on reviewing the past season and looking ahead to the next. It’s a time for rest, reflection, and planning.
The off-season is also the logical time to pause and reflect on our health and make plans as we look ahead. We should be as deliberate about our health planning as we are about next season’s training plan and goals. This is the opportunity to think about (and schedule) our own preventive health maintenance.
Today, I thought we’d talk about serum (in the bloodstream) cholesterol and lipid levels. Please keep in mind that whole books have been written about this topic, so our discussion here will necessarily only cover the essentials. But every athlete should know the essentials!
Why is your cholesterol level important?
As we get older, the problem of atherosclerotic disease (the development of blockages in the body’s arteries that cause heart attack and stroke, or “hardening of the arteries”) becomes more and more important. In fact, cardiovascular disease is responsible for more than one third of deaths in the United States and claims more lives each year than cancer, accidents, diabetes, and chronic lung disease, combined.
I’ve mentioned previously that there are several risk factors for the development of blockages in the coronary arteries, or coronary artery disease (CAD)—and some of these risk factors can be controlled. By you! Your serum cholesterol and lipid levels fit into this category. To review, the other controllable risk factors are: maintaining a normal blood pressure; not smoking; maintaining a healthy body weight; preventing or controlling diabetes; and thankfully for our readers here, being physically active.
It’s estimated that more than one half of adult Americans have a high serum cholesterol level (>200 mg/dL) and as many as 37 million have a very high serum cholesterol level (>240 mg/dL). It’s a big problem.
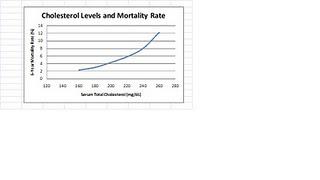
We know from large scale population studies conducted over many years that high cholesterol levels are associated with an increased risk of CAD. That risk isn’t linear, though. Unfortunately, the risk of CAD rises exponentially with increasing levels of serum cholesterol:
Recall from one of my earlier columns about sudden death in athletes that the most common cause of sudden death in athletes older than 30 years is CAD. This set of facts should provide sufficient motivation for even the “healthiest” of athletes to take charge of his own personal situation with cholesterol.
The American Heart Association (AHA) recommends that adults have their serum cholesterol (and other lipids) tested every 5 years. Testing should be performed more often if there are abnormal results, if you have known heart or vascular disease, or if you have 1 or more other major risk factors for CAD.
A Little About Cholesterol and Other Lipids
Cholesterol is a naturally-occurring substance found in the bloodstream and throughout the body. It’s a component of various cell structures, including cell membranes, and serves as a building block for many of the body’s hormones. In these roles, cholesterol is essential. You simply can’t do without it!
We get our cholesterol in 2 ways: 1) we eat it, or 2) our liver makes it. Cholesterol in the diet comes from a variety of sources such as meat, eggs, and dairy products. Importantly, though, even if we didn’t eat ANY cholesterol, the body would still make enough cholesterol to satisfy our body’s needs.
Cholesterol circulates in the bloodstream attached to complex molecules called lipoproteins—molecules that contain both fat and protein. These lipoproteins come in various sizes or densities. The 2 most important forms are: low-density lipoprotein (LDL) and high-density lipoprotein (HDL). Another form of lipid found in the bloodstream is called triglycerides, a slightly different structure made up of 3 fatty molecules held together tightly.
In common parlance, we call LDL the “bad cholesterol” because high levels are associated with an increased risk of CAD. On the flip side, we call HDL the “good cholesterol” because high levels are actually protective against the development of CAD.
When serum cholesterol and LDL levels are high, the excess amounts can be deposited into the walls of the body’s arteries in the form of plaque, leading to narrowing of the blood vessels and the problems of CAD, stroke, or peripheral arterial disease (PAD).
What’s Normal?
Your cholesterol and lipids can be checked at your doctor’s office or a free-standing laboratory. You might consider searching for opportunities for lipid screening programs that are offered as part of community health fairs, often free of charge. You should also check with your employer or insurance company about potentially free lipid screening as a part of various wellness programs in the workplace.
Your most accurate and meaningful test results will come after a period of overnight fasting. If you choose to be tested without fasting and the results are normal, great. If any of the results are high, you should be re-tested after a period of overnight fasting.
The cholesterol and lipid levels are measured in units of milligrams (mg) per deciliter (dL) of blood serum (the liquid component of the blood). Normal ranges have been established by the National Cholesterol Education Program III:
Serum Cholesterol (mg/dL)
Desirable: less than 200
Borderline high: 200-239
High: more than 240
LDL Cholesterol (mg/dL)
Desirable: 100
Near optimal: 100-129Borderline high: 130-159
High: 160-189Very high: more than 190
HDL Cholesterol (mg/dL)
Low: 40
High: more than 60
Triglycerides (mg/dL)
Normal: 150
Borderline high: 150-199
High: 200-499Very high: more than 500
Who Should Get Treated? And How?
If you have high cholesterol or LDL levels, should you be treated? Probably so. The extent of treatment, though, depends upon your overall risk of heart disease. Decisions about drug therapy should only be made with your doctor, who can work together with you to find the best treatment option(s).
All individuals, regardless of their cholesterol or LDL levels, probably benefit from the following therapeutic lifestyle changes (TLC’s):
1. An appropriate diet
a. Saturated fat makes up less than 7% of calories
b. Cholesterol intake less than 200 mg per day
c. Consider increasing viscous (soluble) fiber intake (10-25 g per day)
2. Weight management
3. Increased physical activity
For individuals who already have problems with CAD, stroke, or PAD, the TLC’s should be recommended and drug therapy with a statin medication should be started. The goal of drug therapy is to reduce the LDL level to 70 to 100 mg/dL.
For individuals with 2 or more risk factors for CAD (from among smoking, high blood pressure, low HDL [less than 40 mg/dL], family history of early heart disease, and increased age [men older than 45 years, women older than 55 years]), drug therapy should be considered if TLC’s alone are not successful in reducing the LDL level to less than 130 mg/dL.
For individuals with 0 or 1 of these risk factors, drug therapy should be considered if TLC’s alone are not successful in reducing the LDL level to less than 160 mg/dL.
Many individuals with an elevated serum triglyceride level should also be treated, but the choice of the most appropriate treatment is not as clear-cut and I’d recommend having a discussion with your doctor in this situation.
Some Thoughts About Endurance Athletes and Lipid Levels
Avid endurance athletes are in a fortunate position. Even as little as 30 minutes of exercise daily can result in substantial increases in the serum HDL level which can protect against heart disease. It’s important to remember that in some young, healthy athletes, the total cholesterol level may be relatively high but due primarily to an elevated HDL level that is actually helpful.
Endurance athletes are also likely to be “tuned in” to their diet and can favorably adjust their fat intake to make a difference in their serum cholesterol and LDL levels. Foods that tend to increase the cholesterol level include trans fats and saturated fats (meats, whole milk dairy products, tropical oils, cocoa butter). Foods that tend to decrease the cholesterol level include polyunsaturated fats (nuts, seeds, corn, soybeans, and their oils) and monounsaturated fats (fruits and oils).
Now you’re educated. Take charge and add this to your off-season preventive maintenance checklist.
