The brain fog, dizziness and functional compromise continue to progress despite conservative care. Your doctor referred you for surgical consultation. The surgeon discussed treatment options. What is a Fusion? What is the Occiput? What is the Craniocervical Junction (CCJ)? What is an Occipital Cervical Fusion? What are the indications for an Occipital Cervical Fusion? What are the risks associated with Occipital Cervical Fusion? Are there alternatives to Occipital Cervical Fusion? What is the PICL procedure? Let’s dig in.
What Is a Fusion?
Fusion is a major surgery in which the spine is stabilized by a series of screws, bolts and plates. Fusion surgery can be performed in the neck, thoracic and lumbar spine.
What Is the Occiput?
The Occiput is the back of your skull. Otherwise known as your noggin. The skull resides on top the Cervical Spine. In fact the occiput forms a joint between the base of the skull and the top of the neck that is called the Craniocervical junction. To learn more about this important structure please click here.
What Is the Craniocervical Junction?
The base of the Occiput has a large opening called the Foramen Magnum. Important structures that pass from the skull through the Foramen Magnum include (1):
Spinal Cord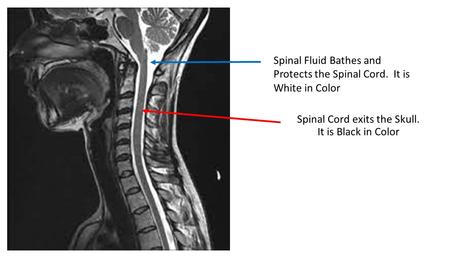
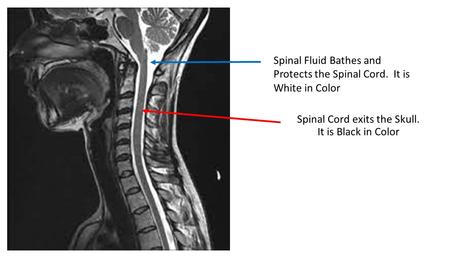
The Spinal Cord consists of neural tissue that starts at the base of the Brain and extends down into the low back. It is a cylindrical bundle of nerve fibers that control our voluntary and involuntary bodily functions. It carries signals between the brain and the rest of the body. As the Spinal Cord descends it is protected on all sides by Spinal bones. These bones provide boney armor to protect against injury. The Spinal Cord has an additional layer of protection afforded by the Spinal Fluid. The Spinal Fluid is also known as Cerebral Spinal fluid. It surrounds the Spinal Cord and extends the entire length of the Spine. The image to the right is a side view of the Spinal Cord as it exits the Brain. The Spinal Cord is black in color. The white that surrounds the Spinal Cord is the Spinal Fluid.
Cranial Nerves
As the Spinal Cord descends through the Foramen Magnum and Spine, important nerves branch off traveling to different parts of the body. There are a large number of nerves. These include the 12 Cranial nerves some of which control muscles whereas others are connected to internal organs such as the heart and lungs.
Arteries and Veins
Arteries and veins provide blood flow to and from important structures in the head, neck, and body. Without blood flow, the body cannot function.
Ligaments
Ligaments are the human duct tape that keeps everything in alignment and stable. The are many ligaments in the neck that provide stability. Two very important ligaments in the upper neck are the Alar and Transverse ligaments. To learn more about these ligaments please click here.
What Is an Occipital Cervical Fusion?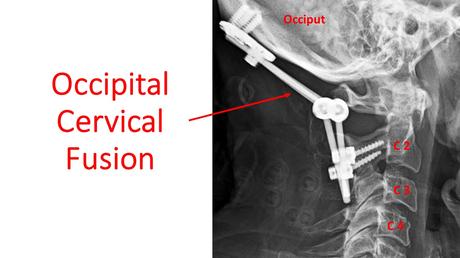
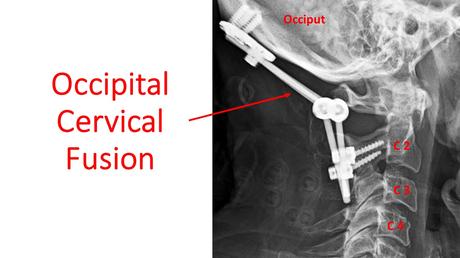
An Occipital Cervical Fusion also known as Occipitocervical Susion is a Major Surgery. It is not a routine operation and is a challenging procedure due to complex anatomy of the upper neck. The procedure involves rods, plates and screws that are placed into the Cervical Spine and Occiput. A plate secured by screws are placed at the base of the Occiput. Screws are also placed into one or more Cervical bones. Rods then connect the Occipital plate to the Cervical screws as shown below. The goal of Occipital Cervical Surgery is a boney fusion between the skull and neck and to relieve any abnormal pressure on the Brain Stem and Spinal Cord.
What Are the Indications for Occipital Cervical Fusion?
Occipital Cervical Fusion is used to treat various disorders of the Craniocervical Junction. The most common indication for Fusion is Craniocervical instability, and Brain Stem/Spinal Cord compression (2).
Craniocervical instability (CCI) is a medical condition where the strong ligaments that hold your head onto your neck are loose or lax (3). The major ligaments involved are the Alar, Transverse and Accessory ligaments. To learn more about CCI please click on the video below.
What Are the Risks Associated with Occipital Cervical Fusion?
The upper Cervical Spine is a very complex area rich in nerves, arteries, veins, ligaments, tendons, and muscles. The risks associated with Upper Neck Fusion are significant and include (4).
Infection
An infection can be localized to the skin or may penetrate deeper into the muscles or bone. Antibiotics are oftentimes required for skin infections. Bone infections require additional surgery.
Screw Loosening
The implanted screw can back out of the bone over time compromising the stability of the upper neck.
Rod/Screw Failure
The screws that are inserted into the Occiput or C1 or C2 as well as the connecting rods can fracture, bend or break. In most cases surgical revision is necessary.
Failed Fusion
Despite the implanted screws and hardware, the Occiput and Cervical Spine may not fuse together. This is called Pseudoarthrosis and compromises the spinal stability.
Cervical Facet injury
A Cervical Facet is a paired joint that resides at each level of the Spine. A poorly placed surgical screw can be advanced into the Facet joint thereby injuring the joint cartilage leading to arthritis, pain, and restriction in range of motion.
Hematoma
A collection of blood that can compress or injure nerves, arteries, and veins.
Nerve Injury
The Upper Cervical Spine is rich in nerves that are susceptible to injury due to traction, cutting of tissue or poorly placed surgical screws.
Continued Pain and Dysfunction
Despite Fusion some patients fail to obtain a reduction in pain and improvement in function.
Vertebral Artery Injury
The Vertebral Artery provides critical blood flow to the Spinal Cord and Brain. The artery can be compressed, irritated, or injured during the surgery.
Dural Leak: The Dura is a thin layer of connective tissue that covers the Brain and Spinal Cord. It can be injured during the surgery resulting in leakage of Spinal Fluid (5).
Limited Neck Range of Motion
Fusion of the Skull Base to the Upper Neck can severely restrict the range of motion in the neck.
Death
Adjacent Segment Disease (ASD): Fusion of the Spine significantly alters the biomechanics of the Spine. The fused segment is no longer able to absorb the forces of daily living. As such these forces are then transferred above and below the Fusion. This additional force can overload the Discs, Facet joints, muscle, and ligaments above and below the Fusion which start to break down. This is called Adjacent Segment Disease. To learn more about this please click on the video below.
Are there Alternatives to Occipital Cervical Fusion?
Yes!
n 2015 a nonsurgical treatment option for Cranial Cervical Instability was developed at the Centeno-Schultz Clinic. It involves the injection of a patient’s own Bone Marrow Concentrate into the damaged Alar and Transverse ligaments. The procedure is for mild to moderate cases of Craniocervical Instability that have not responded to conservative and Upper Cervical injection therapy. The procedure is very demanding and only performed at the Centeno-Schultz Clinic in Broomfield Colorado. The procedure is called Percutaneous Implantation of Cervical Ligaments (PICL) To learn more about this groundbreaking procedure please click on the video below.
In Summary
Fusion is a major surgery in which the Spine is stabilized by a series of screws, bolts and plates.
The Occiput is the back of your skull.
The Craniocervical Junction is where the Occiput and the Upper Neck bones come together to form a joint.
The Craniocervical Junction contains vital structures that include the Spinal Cord, Cranial Nerves, arteries, veins and ligaments.
An Occipital Cervical Fusion is a major surgery that involves screws, plates and rods that are placed into the Upper Cervical Spine and Occiput.
Occipital Cervical Fusion is used treat various disorders of the Craniocervical Junction. The most common indication is Craniocervical Instability (CCI) and Brainstem/Spinal Cord compression.
The risks associated with Occipitocervical Fusion are significant and include:
- Infection
- Screw Loosening
- Rod/Screw Failure
- Failed Fusion
- Cervical Facet Injury
- Hematoma
- Continued Pain and Dysfunction
- Vertebral Artery Injury
- Dural Leak
- Limited Range of Motion
- Adjacent Segment Disease
Percutaneous Implantation of Cervical Ligaments (PICL) is an non surgical treatment option for mild to moderate cases of Craniocervical Instability that have not responded to conservative care.
If you or a loved one continue to suffer from headaches, dizziness, brain fog and chronic fatigue that has not responded to conservative therapy please schedule a telemedicine consultation. A board certified, fellowship trained Physician will review your history, imaging and discuss appropriate treatment options.
1.Flanagan MF. The Role of the Craniocervical Junction in Craniospinal Hydrodynamics and Neurodegenerative Conditions. Neurol Res Int. 2015;2015:794829. doi:10.1155/2015/794829
2.Deutsch H, Haid RW Jr, Rodts GE Jr, Mummaneni PV. Occipitocervical fixation: long-term results. Spine (Phila Pa 1976). 2005 Mar 1;30(5):530-5. doi: 10.1097/01.brs.0000154715.88911.ea. PMID: 15738785.
3.Offiah CE, Day E. The craniocervical junction: embryology, anatomy, biomechanics and imaging in blunt trauma. Insights Imaging. 2017;8(1):29–47. doi:10.1007/s13244-016-0530-5
4.Kukreja S, Ambekar S, Sin AH, Nanda A. Occipitocervical Fusion Surgery: Review of Operative Techniques and Results. J Neurol Surg B Skull Base. 2015;76(5):331-339. doi:10.1055/s-0034-1543967.
5.Upadhyaya M, Jain S, Kire N, Merchant Z, Kundnani V, Patel A. Surgical, clinical, and radiological outcomes of occipitocervical fusion using the plate-screw-rod system with allograft in craniocervical instability. J Craniovertebr Junction Spine. 2019;10(4):216-223. doi:10.4103/jcvjs.JCVJS_87_19

