While preparing for the group activities or quizzes for the GHHM Course, we come across a lot of disease conditions, and one of the strategies that I tried to adopt was to create short notes on the individual diseases, as well as study up the public health approach to prevent and control epidemics or outbreaks of these diseases. So, for example, the disease under discussion for the week was Diphtheria; I would create a short summary about the disease, and write out a short note on the management of an outbreak of diphtheria. Whilst the disease profile was a little more detailed, usually running to 3-4 pages of hand written notes, the outbreak management was seldom more than 1.5 pages long, and oriented to something that I could write for the test. Unfortunately, I started this process quite late in my preparation and could not adopt this approach for all conditions being tested or discussed. It would have been helpful to have done this for more conditions and keep myself more exam-ready. Here is the disease profile for Diphtheria. Please note that I cannot be held liable for any mistakes in these notes, and you should refer to an authoritative textbook, and not random internet blogs, for your information.
Background
- Caused by Corynebacterium diphtheria: aerobic, gram positive bacillus
- Toxin production occurs when infected with phage with tox gene; potent toxin
 Corynebacterium diphtheriae<\/i> bacteria, which had been stained using the methylene blue technique. The specimen was taken from a Pai\u0092s slant culture.\r\rDiphtheria is an acute bacterial disease caused by toxigenic strains of Corynebacterium diphtheriae<\/i> and occasionally C. ulcerans<\/i>. It is transmitted through respiratory droplets and personal contact. Diphtheria affects the mucous membranes of the respiratory tract, known as \u0093respiratory diphtheria\u0094, the skin, termed \u0093cutaneous diphtheria\u0094, and occasionally other sites including the eyes, nose, or vagina. Diphtheria remains a serious disease throughout much of the world. In particular, large outbreaks of diphtheria occurred in the 1990s throughout Russia and the other former Soviet republics. Most life-threatening cases occurred in inadequately immunized persons. Travelers to disease-endemic areas are at increased risk for exposure to toxigenic strains of C. diphtheriae<\/i>.","created_timestamp":"0","copyright":"","focal_length":"0","iso":"0","shutter_speed":"0","title":"","orientation":"0"}" data-large-file="https://scepticemia.files.wordpress.com/2019/07/corynebacterium-diphtheriae.jpg?w=585" />Corynebacterium diphtheriae (Image Credit: Isis325 Flickr)
Corynebacterium diphtheriae<\/i> bacteria, which had been stained using the methylene blue technique. The specimen was taken from a Pai\u0092s slant culture.\r\rDiphtheria is an acute bacterial disease caused by toxigenic strains of Corynebacterium diphtheriae<\/i> and occasionally C. ulcerans<\/i>. It is transmitted through respiratory droplets and personal contact. Diphtheria affects the mucous membranes of the respiratory tract, known as \u0093respiratory diphtheria\u0094, the skin, termed \u0093cutaneous diphtheria\u0094, and occasionally other sites including the eyes, nose, or vagina. Diphtheria remains a serious disease throughout much of the world. In particular, large outbreaks of diphtheria occurred in the 1990s throughout Russia and the other former Soviet republics. Most life-threatening cases occurred in inadequately immunized persons. Travelers to disease-endemic areas are at increased risk for exposure to toxigenic strains of C. diphtheriae<\/i>.","created_timestamp":"0","copyright":"","focal_length":"0","iso":"0","shutter_speed":"0","title":"","orientation":"0"}" data-large-file="https://scepticemia.files.wordpress.com/2019/07/corynebacterium-diphtheriae.jpg?w=585" />Corynebacterium diphtheriae (Image Credit: Isis325 Flickr)Epidemiology
- Reservoir: Human carriers, usually asymptomatic
- Transmission: person-to-person via respiratory tract secretions; rarely from skin and fomites
- Seasonal trends in disease burden seen; higher case counts in winter or spring
- Transmissibility: Untreated cases may cause transmission for 2-4 weeks; chronic carriers shedding >6 months documented. Effective antibiotic therapy eradicates carriage
- Extremely rare in developed countries; major burden from: India, Haiti, Nigeria, Brazil
- Recent outbreaks in FDMN refugee camps in Cox’s Bazar, Bangladesh
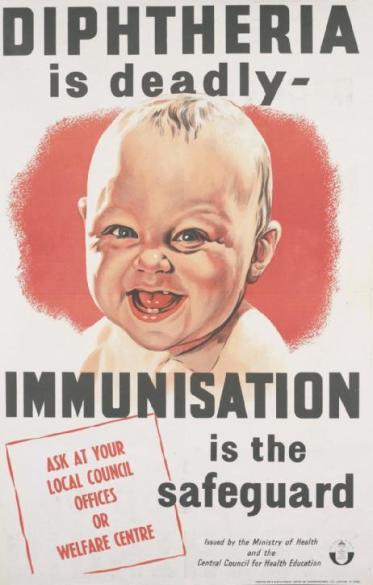
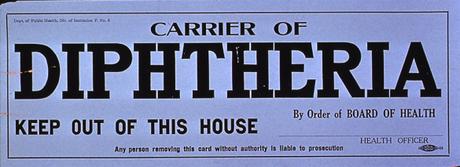 Image Credit: NIH NLM Visual Culture and Public Health Posters
Image Credit: NIH NLM Visual Culture and Public Health PostersClinical Presentation
- Incubation period 2-5 days; may affect any mucus membrane
- Presentation and clinical classification depends on affected site:
- Anterior Nasal: like common cold; mucopurulent nasal discharge which then becomes blood tinged
- Pharyngeal/Tonsillar: most common site; insidious pharyngitis with fever; membrane – bluish-white (2-3 days) à greyish green or black if bleeding (4-5 days); firmly adherent pseudomembrane, bleeds on manipulation. Extensive membranes can obstruct respiration. Severe disease: submandibular and anterior neck edema (bull neck); very toxic presentation
- Laryngeal: Extension of pharyngeal diphtheria; fever, hoarseness, barking cough; airway obstruction by membrane
- Cutaneous: Often in homeless people. Scaling rash, or ulcers with clearly demarcated edges and membrane.
- Complications: Attributable to toxin; most common – myocarditis, neuritis; early myocarditis often fatal, causes arrhythmia. Paralysis of soft palate most common neurologic complication. Often resolves completely. Diaphragmatic palsy may cause pneumonia and consolidation.
- Case Fatality Rate: Overall 5-10%; higher in extremes of age, maybe 20%.
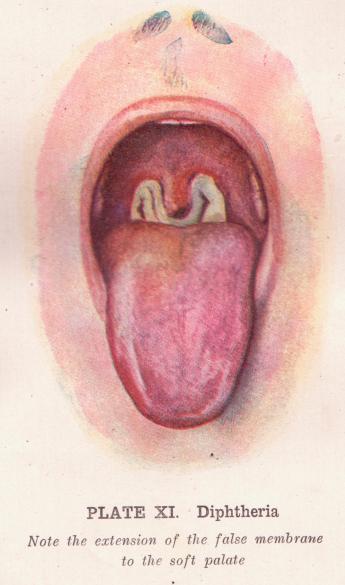 Image Credit: Sue Clarke on Flickr
Image Credit: Sue Clarke on FlickrDifferential Diagnosis
Differential diagnosis of neck swelling and membranous pharyngitis include the following
- Group A Beta Hemolytic Streptococcus
- Staphylococcus aureus
- Arcanobacter hemolyticum
- Candida albicans
- Borrelia vincenti (Vincent’s angina)
- Haemophilus influenzae (Acute epiglottitis)
- Epstein-Barr virus (EBV) (Infectious mononucleosis)
- Adenovirus
- Herpes simplex
- Rare presentation: Toxoplasma spp
- Fusobacterium necrophorum (Lemierre’s syndrome)
- Non-communicable cause: Methotrexate; steroid therapy leading to oral candidiasis
Diagnosis
- Often only clinical diagnosis; lab diagnosis may take too much time. Presumptive treatment initiated earliest
- Suspected case: Pharyngitis, naso-pharyngitis, tonsillitis, laryngitis, tracheitis (or any combination of these), absent or low grade fever Grayish adherent pseudo-membrane present; membrane bleeds, if manipulated or dislodged.
- Probable case: Suspect case above + 1 or more of the following
- Stridor
- Bull-neck (cervical edema)
- Toxic circulatory collapse
- Acute renal insufficiency
- Sub-mucosal or sub-cutaneous petechiae
- Myocarditis
- Death
- Epidemiological linkage:
- Recently returned (<2 weeks) from travel to area with endemic diphtheria?
- Recent contact (<2 weeks) with confirmed diphtheria case or carrier?
- Recent contact (<2 weeks) with visitor from area with endemic diphtheria?
- Recent contact with dairy or farm animals? Domestic pets?
- Immunization status: Up-to-date – any DTaP/DT/Tdap/Td shot within past 10 years?
- Laboratory Confirmed Case:
- Positive culture of C. diphtheriae (or C. ulcerans) AND – Positive Elek Test; OR
- PCR for tox gene (Positive for subunit A and B)
Treatment
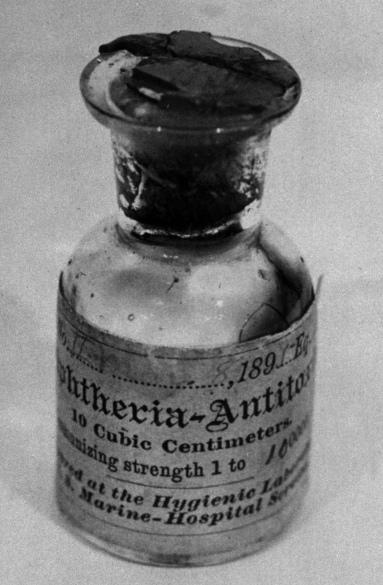
- Diphtheria anti-toxin
- DAT should be administered immediately to probable cases with respiratory diphtheria
Severity of diphtheria Dosage for adults and children
Laryngeal or pharyngeal of 2 days duration 20,000-40,000 IU
Nasopharyngeal disease 40,000-60,000 IU
Extensive disease of 3 or more days of duration or any patient with diffuse swelling of the neck (respiratory distress, hemodynamic instability) 80,000-100,000 IU
- Antibiotic therapy
- For severely ill patients:
- Procaine benzyl penicillin (penicillin G): IM 50 mg/kg once daily. Treat for total 14 days.
- Aqueous benzyl penicillin (penicillin G): administer IM or slow IV All persons: 100,000 units/kg/day administer in divided dose of 25,000 IU/kg every 6 hours.
- IV Erythromycin: 40-50 mg/kg/day (maximum, 2 gm/day). Administer in divided doses, 10- 15 mg/kg every 6 hour, maximum 500 mg per dose. Treat for total 14 days.
- For patients who can swallow and are less ill, use oral preparation.
- Oral phenoxymethylpenicillin V All persons: 50 mg/kg/day, in divided doses 10-15 mg/kg/dose administered every 6 hours. Maximum is 500 mg per dose. Treat for 14 days.
- Oral erythromycin: 40-50 mg/kg/day (maximum, 2 gm/day). Administer in divided dose, 10- 15 mg/kg every 6 hour, maximum 500 mg per dose. Treat for total 14 days.
- Oral azithromycin: For children: 10-12 mg/kg once daily (max. 500 mg/day). Treat for total of 14 days. For adults: 500 mg once daily. Treat for total of 14 days.
- For severely ill patients:
- Supportive therapy
- Monitor the patient closely
- Manage shock
- Supportive therapy: Paracetamol for fever; supportive therapy for myocarditis, neuritis or other complications
- Care of close contacts
- Vaccination: Number of doses: Only one dose if documentary evidence of having completed primary; otherwise, three doses: at least 4 weeks’ interval between each dose.
- Antibiotics for prophylaxis.
- IM benzathine penicillin: a single dose for children aged ≤ 5 years: administer 600,000 units; for those > 5 years: administer 1,200,000 units
- Oral erythromycin for children: 40 mg/kg/day, administered in divided doses, 10 mg per dose, every 6 hours; For adults: 1 g/day, administered in divided doses, 250 mg per dose every 6 hours Treat for total 7 days
- Oral Azithromycin Children: 10-12 mg/kg once daily, to a max of 500mg/day. Treat for total 7 days Adults: 500mg once daily. Treat for total 7 days.
- Exclude from school or work until 48 hours of antibiotics have been completed