The neck pain started out gradually but continued despite conservative care and medications. Your doctor referred you for a surgical consultation. What is Cervical Fusion? Are there different types of Cervical Fusions? What happens during surgery? What are the indications for Neck Fusion surgery? What is the recovery from Neck Fusion? What are the complications associated with Cervical Fusion? What are the alternatives to Cervical Fusion? What regenerative alternatives exist?
Cervical Fusion: Introduction
Cervical Fusion is often recommended when chronic neck pain problems worsen over time. What exactly is it?
Cervical Fusion is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back( posterior) of the Cervical spine. The disc between the spinal bones is often times removed and replaced with a bone graft or a spacer.
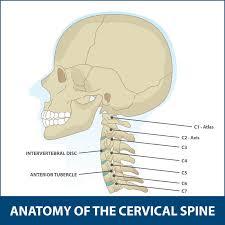
The neck of composed of 7 boney building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the Cervical Spine. Hence the bones in the neck are C1 through C7. Sandwiched between neck bones are important shock absorbers called Discs. A Cervical Fusion surgery removes this important shock absorber and joins the adjacent bones together with hardware.
Find out if Cervical Fusion is the right procedure for you. This post will cover the types of Cervical Fusion and indications.
Types of Cervical Fusion Procedures
There are several different types of Cervical Fusion procedures. The differences in part are due to their approach to the Cervical Spine. The two most common Cervical Fusions are an Anterior Cervical Discectomy (ACDF) and a Posterior Fusion. The goal is the treat symptomatic neck conditions that are progressive in nature and have not responded to conservative therapy. The Disc is removed in an effort to decrease the pain and relieve exiting nerve root or Spinal Cord compression. The principal difference between these two surgeries is the approach to the spine. One is from the front (anterior) whereas the other is from the back (posterior).

Anterior Cervical Discectomy and Fusion (ACDF) Interbody Fusion
This is one of the most common type of neck surgeries. One study cited an average of 137,000 ACDF surgeries performed annually in the United States (2). It involves removing the Disc through the front of the neck followed by the insertion of a plate with screws to stabilize the spine.

Posterior Fusion
A Posterior Fusion surgery involves removing the Disc from the backside of the neck. The surgical approach is from the posterior. Access to the Disc is more difficult through a posterior approach. Accordingly, there are significant postoperative complications with this approach that range from 8.6-49% (3)
What Happens During the Surgery?
Cervical Fusion is performed at a hospital or outpatient surgical center. It involves a general anesthetia in which you are put to sleep for the duration of the surgery.
Anterior Cervical Discectomy and Fusion has four principal steps.
Step 1: Anterior surgical approach
Anterior refers to the front of the neck. A horizontal skin incision is made in the front of the neck followed by separation of the different layers of muscle, tendons and fasica.
Step 2: Removal of Disc AKA Discectomy
After the correct Cervical Disc is identified using x-ray, it is surgically cut out. This removes the problematic Disc and allows evaluation of deeper structures in the Cervical Spine.
Step 3: Decompression of the Cervical Canal
Once the Disc in removed, the Posterior Longitudinal Ligament (PLL) is identified. This stabilizing ligament is frequently trimmed or cut out to allow for visualization of the central spinal canal. If an extruded Disc, Disc fragments or bone spurs are present within the Central Canal, and they are surgically removed. In addition, the boney doorway through which the spinal nerves exits is evaluated and roto-rootered out if bone spurs are compressing or irritating the spinal nerves.
Step 4: Cervical Fusion
A surgical cage or implant along with a bone graft is then inserted into the space previously occupied by the Cervical Disc. The goal is to maintain the disc space height and promote the two Cervical bones to mend together. A small plate is then attached in the front of the neck to the cervical bones. It provides stability and promotes fusion of the two bones.
Indications for Neck Fusion Surgery
There are several Cervical Spine conditions that may require surgery. The most common include:
Cervical Disc Degeneration/Injury
The Disc a important shock absorber that is sandwiched between the spinal bones in the neck. It is susceptible to injury and degeneration as result of trauma, and repetitive wear and tear. One or more Discs may become a source of severe neck pain. When conservative treatments fail some patients are referred for Cervical Fusion surgery.
Cervical Spinal Instability
The neck is composed of 7 bones stacked upon one another. They are held in place by ligaments, muscles, tendons, and fascia. If any of these structures are weakened or injured one of more of the stacked bones can slip forward. This is called Anterolisthesis. If the bone slips backwards in relation to the other bones, it is called Retrolisthesis. This movement can cause significant irritation and or injury to the Spinal Cord, exiting nerve roots, Facet joints and Cervical Discs. This in turn can cause debilitating neck and upper extremity pain. When it involves the ligaments that hold the head onto the neck patients can suffer significant neurologic symptoms including brain fog, fatigue, headaches, visual problems and vertigo. This condition is known as Craniocervical Instability (CCI). To learn more about Craniocervical Instability please click on the video below.
Nerve Compression
Nerves exit the Cervical Spine through a boney doorway called the Neural Foramen. The Foramen can be narrowed by Disc protrusion, Disc herniation, Facet joint overgrowth, ligament instability, Disc slippage or a cyst causing compression or injury to the nerve. This can cause radiating arm and hand pain, numbness and tingling and reduced muscle strength. When unresponsive to conservative care, some patients are referred for Neck Fusion evaluations.
Spinal Cord Compression
The Spinal Cord is the nerve network that controls most of your body’s function. It starts at the base of the brain and extends into the low back. It is encased in a protective layer of bone. It is surrounded and protected by an additional layer of fluid called the Cerebral Spinal Fluid. The Spinal Cord is fragile and susceptible to injury. Symptoms can be mild or severe depending on the extent of the damage. A tragic example is that of Christopher Reeves who sustained a traumatic Spinal Cord injury after a falling from a horse. He was paralyzed and required assistance with all bodily functions including breathing.
Trauma to Cervical Spine
Trauma to the spine can cause instability, compression of nerves and discs. Cervical Fusion is often recommended in severe cases to stabilize the spine and avoid Spinal Cord injury and paralysis.
Infection
The Cervical bones and Disc can become infected causing significant damage the neck. Neck Fusion is a treatment option when the infection is not controlled with antibiotic therapy.
Tumors
Cancer can occur anywhere in the body. When it occurs in the neck it can compromise the Spinal Cord, exiting Spinal nerves and the Discs. When the integrity of the Spine is compromised and conservative treatments fail, Cervical Fusion is often recommended.
Recovering From Neck Fusion Surgery
Recovery Time
Recovery time can vary widely from patient to patient. Factors affecting recovery time include severity of neck injury, activity level prior to the Neck Fusion and number of Cervical levels fused. Surgical pain typically improves in 1-3 weeks. Physical therapy is essential after the surgery and is typically started 3-4 hours after the surgery. The goal is provide strengthening and improve range of motion.
Eight Potential Complications Associated with Neck Fusion
There are inherent risks associated with any surgery. The most common complications from a Cervical Fusion include:
Difficulty Swallowing

Difficulty swallowing is called Dysphagia and can occur after Neck Fusion. The incidence of dysphagia after Cervical Fusion Surgery in one study was 12.7% (4). Difficulty swallowing can compromise calorie, fluid intake, and healing.
Failed Fusion
This is BAD news. Failure of the bones to fuse is called Non-union or Pseudoarthrosis. It means that despite the surgery, the inserted screws and plates, the extensive rehabilitation, and the pain the bones did not fuse together. The intended surgery has failed and now there is instability in the neck. The incidence of Non-union is striking and in one study was found to be 52% (5). The treatment for Non-union is terrible as it involves another surgery where the Fusion is revised and oftentimes the fusion is extended up or down an additional level.
Continued Neck Pain

Despite Neck Fusion surgery, many patients continue to have ongoing neck pain that requires oral narcotics. In a recent study 1 year after neck fusion only 39% of patients were able to return to work (6).
Spinal Fluid Leak (CSF)
The Dura is the outermost membrane that covers the Brain and Spinal Cord. This important membrane can be punctured during surgery causing a leak of Spinal Fluid. The incidence ranges from 1-17% (7). Severe headache is a common symptom of Spinal Fluid Leak. If left untreated, a Spinal Fluid Leak (CSF) can lead to infection, Brain abscess, and bleeding.
Nerve Injury
Nerves can be damaged during surgery and the incidence varies from 0.18% to 2.6% (8). Nerve injury can include exiting nerves as well as the spinal cord itself. After Cervical Fusion surgery patients may awaken after surgery with new onset left arm, face, or lower extremity pain.
Changes in Spinal Curve
The natural C curve in the neck is important for optimal function as it ensures proper alignment of all the bones, tendons, and ligaments in the neck. Cervical Fusion surgery not only alters the natural C curve in the neck but also adversely affects the curve in the low back. Ouch! A new study demonstrated that patients who underwent Cervical Fusion noted changes in both the neck, tailbone, and pelvis curves. This oftentimes leads to the onset of pain and injury (9).
Infection

Infection is a devastating complication and was found to occur in 16.6% of patients in a recent study. (10). Infection can involve the skin, muscle or bone. Treatment involves antibiotics, wound care, and 47% of patients in a recent study required additional surgery for wound care and skin grafting.
Adjacent Segment Disease
Adjacent Segment Disease (ASD) is a common complication of Neck Fusion with an incidence of 21% (11). It occurs as a direct result of the Fusion surgery. Why? The neck Discs are designed to absorb the forces of daily living. Fusing one or more discs together results in additional forces being placed on the Disc and Facet joints above and below the Fusion. This additional pressure results in wear and tear and degeneration often times requiring additional surgery. See our video below:
Alternatives to Cervical Fusion
There are several non-surgical treatment options for ongoing neck and arm pain. The appropriateness and success of these treatment options is based upon the severity of the injury, current symptoms and co-existing medication conditions. The most common treatments include:
Conservative Care
Conservative care when appropriate is the first line treatment for neck and arm pain. Treatment options include rest, stretching, physical therapy, and chiropractic care. The goal is to reduce ongoing pain and increase function.
Medications
Medication is often used in conjunction with conservative care. Examples include anti-inflammatory agents and muscle relaxants. Oral steroids are often recommended when pain persists but should be avoided due to the significant side effects including destroying cartilage, depressing stem cell activity and altering sugar levels. To learn more about the adverse effects of steroids please click here.
Traditional” Pain” Injections
When medication and conservative care fail, patients are often referred to a pain clinic for injections. These are STEROID injections and should be avoided. Steroids are powerful ant-inflammatory agents with many side effects detailed above. Furthermore, they can accelerate the underlying problems. Steroids cannot heal an injured Disc or Facet joint. Steroids can only decrease the inflammation associated with the injury. Healing of a neck injury requires a Regenerative option.
Regenerative Alternatives to Cervical Fusion
The Centeno-Schultz Clinic are experts in the treatment of neck pain. We are also experts in the use of PRP and Bone Marrow Concentrate in the spine. In 2005 we become the first clinic in the world to inject Bone Marrow-derived stem cells into the Disc. We are also leaders in the field of Regenerative Medicine and Interventional Orthopedics. We have published extensively in recognized, peer-reviewed journals. Our list of publications is available here.
Our approach is much different. Unlike the rushed, brief exam in most Orthopedic offices, we spend a dedicated amount of time reviewing your chief complaint, its duration, aggravating and alleviating factors, treatment to date, past medical history, medications, and events that led to the injury. We also review in detail all imaging. This includes x-ray, MRI, and CT scans.
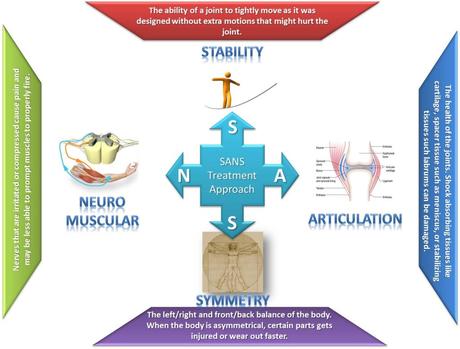
Our approach is comprehensive in nature as we believe the body functions as a unit. For example examination of the shoulders is critical when evaluating patients with neck pain. This is because many patients with low Neck pain also have ongoing shoulder problems. The approach is referred to as SANS which stands for: Stability, Articulation, Neuro-Muscular and Symmetry. To learn more about our SANS approach please click here.
At the Centeno Schultz Clinic, there are an extensive number of Regenerative treatment options for patients with ongoing neck and or arm pain. The specific treatment will depend upon the underlying cause of the pain, its severity, and the patient’s symptoms. Treatment options include both PRP and Bone Marrow Concentrate which contains stem cells. We utilize customized PRP injections to ensure the best clinical results. It is important as middle aged and older patients require higher concentrations of PRP than younger patients. To learn more about the importance of PRP concentration please click here.
Both Bone Marrow Concentrate and PRP are precisely injected into the neck using x-ray and ultrasound guidance. The injections are challenging and cannot be performed by your surgeon, chiropractor, or physician assistant. To watch a Centeno-Schulz Clinic injection click on the video below.
In Conclusion
- Cervical Fusion is a major surgery that involves joining one or more of the Spinal bones together using screws, bolts and plates.
- The two most common Cervical Fusion procedures include the Anterior Cervical Discectomy and Fusion (ACDF) and Posterior Fusion.
- ACDF involves four principal steps which are described above.
- The most common indications for Neck Fusion are Disc degeneration, Cervical instability, nerve compression, Spinal Cord compression, trauma, infection and tumors
- Recovery time from Neck Fusion surgery varies depending upon multiple factors
- The eight potential complications associated with Cervical Fusion surgery include difficulty swallowing, failed fusion, continued neck pain, Spinal Fluid Leak, nerve injury, changes in spinal curve, infection, and Adjacent Segment Disease.
- Alternatives to Cervical Fusion include when appropriate conservative care, medications and traditional pain injections.
- Steroids are powerful ant-inflammatory agents that are associated with significant side effects and only treat the inflammation and NOT the underlying problem.
- Regenerative treatment options identify and address the underlying problems utilizing a comprehensive approach and targeted injections using ultrasound and x-ray.
- PRP and Bone Marrow Concentrate are powerful treatment options for neck and arm pain.
If you or a loved one continue to suffer from neck and or arm pain that has not responded to conservative therapy please schedule a telemedicine consultation. A board certified, fellowship trained physician will review your history, imaging and discuss appropriate treatment options.
1.Srikhande NN, Kumar VAK, Sai Kiran NA, et al. Clinical presentation and outcome after anterior cervical discectomy and fusion for degenerative cervical disc disease. J Craniovertebr Junction Spine. 2019;10(1):28-32. doi:10.4103/jcvjs.JCVJS_87_18
2.Epstein NE. A Review of Complication Rates for Anterior Cervical Diskectomy and Fusion (ACDF). Surg Neurol Int. 2019;10:100. Published 2019 Jun 7. doi:10.25259/SNI-191-2019
3.Badiee RK, Mayer R, Pennicooke B, Chou D, Mummaneni PV, Tan LA. Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. J Spine Surg. 2020;6(1):323-333. doi:10.21037/jss.2019.11.01
4.De la Garza-Ramos R, Xu R, Ramhmdani S, Kosztowski T, Bydon M, Sciubba DM, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A. Long-term clinical outcomes following 3- and 4-level anterior cervical discectomy and fusion. J Neurosurg Spine. 2016 Jun;24(6):885-91. doi: 10.3171/2015.10.SPINE15795. Epub 2016 Feb 19. Erratum in: J Neurosurg Spine. 2016 Jun;24(6):996. PMID: 26895527.
5.https://medicalxpress.com/news/2018-10-pseudarthrosis-single-level-acdf-peek-interbody.html
6. Faour M, Anderson JT, Haas AR, et al. Return to Work Rates After Single-level Cervical Fusion for Degenerative Disc Disease Compared With Fusion for Radiculopathy in a Workers’ Compensation Setting. Spine. 2016;41(14):1160-6.DOI: 10.1097/BRS.0000000000001444.
7.Tosun B, Ilbay K, Kim MS, Selek O. Management of Persistent Cerebrospinal Fluid Leakage Following Thoraco-lumbar Surgery. Asian Spine J. 2012;6(3):157-62. doi: 10.4184/asj.2012.6.3.157.
8.Cheung JP, Luk KD. Complications of Anterior and Posterior Cervical Spine Surgery. Asian Spine J. 2016;10(2):385-400.doi: 10.4184/asj.2016.10.2.385
9.Cheung JP, Luk KD. Complications of Anterior and Posterior Cervical Spine Surgery. Asian Spine J. 2016;10(2):385-400.doi: 10.4184/asj.2016.10.2.385
10.Barnes M, Liew S. The incidence of infection after posterior cervical spine surgery: a 10 year review. Global Spine J. 2012;2(1):3-6.doi: 10.1055/s-0032-1307252.
11.Wu XD, Wang XW, Yuan W, et al. The effect of multilevel anterior cervical fusion on neck motion. Eur Spine J. 2012;21(7):1368-1373. doi:10.1007/s00586-012-2157-7

