
Michael in the ICU
on a BIPAP Machine
Even though my husband Michael has never* had any respiratory problems, he was hospitalized for 14 days this month because he had a severe case of community-acquired [bacterial] pneumonia.
*Yes, he had pneumonia before--but he was only 9, and he was not hospitalized for it.
From Sunday 03 February to Saturday 17 February, my husband spent eight days in the intensive care unit and six days in a regular hospital room. These were two hospital stays because he was discharged on Saturday 10 February and spent about 30 hours at home (Saturday 10 February 12:30 pm to Sunday 11 February 4:30 pm) before requiring readmittance.
I was initially calm, but when he returned the second time, it was a bit more unsettling.
Note: This post does not convey medical advice. Its purpose is to raise awareness. If you have any questions about your respiratory system, please see a licensed medical professional.
The First Visit
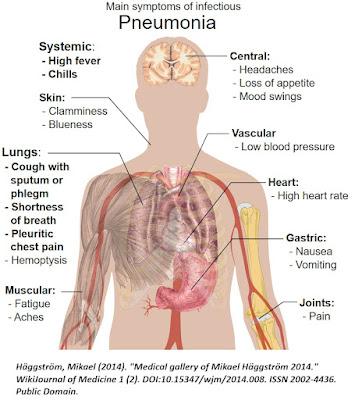
Michael's main symptom was fatigue. He was sleeping a lot. He did have a low-grade fever, but he was not coughing; he did not complain of shortness of breath. He did not show signs of low oxygen (blue lips, blue fingernail beds). He was primarily sleeping a lot. We checked his blood pressure and temperature, and then I decided to go buy an oximeter since I could not find our since we were still unpacking from our move.
I am glad that I bought the oximeter. His blood oxygen level was 70% when it's supposed to be in the high 90s. If you do not own an pulse oximeter, I highly suggest that you buy one for home use.
How to Use a Pulse Oximeter to Check Oxygen Saturation Levels
We took him to our little rural hospital in Mount Pleasant, Utah where he tested negative for COVID-19, RSV, Influenza A and Influenza B. They also did a CT scan looking for a pulmonary embolism. Additionally, the did an EKG to exclude heart problems. The person supervising his care was a physician assistant; however, they did a teleconference with an MD out of St. George, Utah. She was looking for heart problems via on-site imaging and blood tests, but they could never find a heart problem.
Our rural hospital did not have the equipment to deliver oxygen at a rate that would raise his blood oxygen saturation level into the 90s, so they transferred him by helicopter north by two counties (about 78 miles from our house). Both Michael and I did not think this was necessary (at $1,500 per minute), but we did not argue with the medical professionals.
Lifeflight Helicopter Outside of
Utah Valley Regional Hospital in Provo, Utah
Once he got to Utah Valley Regional Hospital, he went through more testing (duplicating some of the tests done in Mount Pleasant). They put him on a BIPAP machine and delivered broad spectrum antibiotics. They took some samples to send to the lab to grow a culture in hopes of specifically identifying the bacteria. These cultures never grew anything definitive.
Friends and relatives repeatedly asked how he caught pneumonia, but the doctors could never determine this. Here is a page hosted by the Cleveland Clinic that gives a great general overview on pneumonia.
Michael's oxygen would dip if he laid down, so he had to have his bed in an upright position (no greater than a 45 degree angle). He was able to move from the BIPAP to a CPAP after a few days, but even after returning home, he still sleeps at a 45 degree angle in a recliner. He transitioned to a regular cannula with oxygen for his last two days in the hospital.
Michael was eager to get home so that he could do some work in his home office, so they discharged him on Saturday 10 February with a script for oral antibiotics, an oxygen concentrator, and four oxygen tanks for travel outside of the home (i.e., doctor visits).
That was a mistake. He relapsed the next day after going 22 hours between intravenous antibiotics and his first dose of oral antibiotics. During those 22 hours, the bacteria roared back into his lungs, dropping his oxygen again.
Apparently, about 10% of patients with bacterial pneumonia need an additional day of intravenous antibiotics. Michael was the statistical outlier.
The Second Visit
Michael seemed to be in recovery, so on Sunday I went to church for an hour. I then came home and fed him lunch. Again, he seemed to be doing fine, so I returned to church to visit with the congregational leader about a temple recommend.
Just as I finished that interview, I got a text with a photo from Michael. The text read "Help." The photo showed a reading on his pulse oximeter of 60%. I ran out of there in my three-inch heels. Thankfully, the church building is only 500 yards from our house.
When I got home, I found out that he actually had a reading of 55% at one point, but he was shaking so hard that he couldn't get a photo of that. He was chattering and shaking. He had a mild fever again. He looked sicker this time than he did the first time when he was only sleepy. It was alarming.
We tried to determine if the low reading was due to our improper use of the equipment. Consequently, Michael and I switched him from the concentrator to the oxygen tank. We also changed the tubing and cannula. I even went to the store to buy a glucose monitor to see if he was shaking from low blood sugar. I had him on the phone during my trip to the store, asking him every minute to tell me if he was still conscious.
We were in denial that he was relapsing and probably should have gone to the hospital immediately. However we spent from about 1:30 pm to 3:30 pm trying to ensure that the problem wasn't our inability to manage him correctly.
We drove north from our house to Mount Pleasant (about 15 miles) to the rural hospital again. The local medical team worked on him until about 8 pm. Again, they could not get his blood oxygen saturated into the 90s. (They just don't have the right equipment.) Consequently, they took him by ambulance back to the regional hospital in Provo.

Michael and His Medical Team
Starting the Transport by Ambulance
Well, we knew the drill with this second visit.
The doctors did run new tests to exclude something in the house that might be making him sick, so they tested for mold, Legionnaire's disease and other common household dangers. They all came back negative. Again, they took a culture that never grew anything during his second 7-day visit. Again, he went from BIPAP to CIPAP to a regular cannula.
Finally, he was discharge on Saturday 17 February with the expectation that he will be on supplemental oxygen for about six weeks. We are hoping that the antibiotics really defeated the bacteria this time.
All my best to anyone battling pneumonia. This was the first time that Michael has ever been hospitalized in his life. Even though about 10% of people who are hospitalized for pneumonia have a relapse within two years, we are hoping that he is part of the 90% for those statistics.

