The lumbar section of the spine is an extraordinarily resilient and complex structure, responsible for enabling everyday movement, supporting and redistributing loads, and protecting the spinal nerve. But despite how much we rely on our lower back in our daily lives, we tend to notice how much our lumbar spine does for us only when we suffer an injury.
Lower back injuries may not be life-threatening – but can be severe enough to impair mobility, cause chronic pain, and lead to withdrawal from sports and activities. Studies also tell us that lower back pain is a significant risk factor for declining mental health, depression, and anxiety.
Fortunately, this downward spiral can be halted – or prevented altogether – without pain medications or surgery. Our research-based regenerative approach leverages the potential of orthobiologics to provide patients with L3 pain an alternative to invasive or pharmaceutical intervention. Discover more below.
Anatomy of the L3
The lumbar spine – or lower back – consists of five vertebrae (a small percentage of people have six). A vertebra is a small, cylindrical bone with an arched (ring-like) component, called the vertebral arch, responsible for safeguarding the spinal cord.
The vertebrae are the building blocks of the spine and play an essential role in providing structural support, facilitating flexibility and motion, and protecting the spinal cord.
The vertebrae in the lower back are numbered L1 to L5, where “L” stands for lumbar:
- L1. This is the first lumbar vertebra, located where the thoracic spine ends.
- L2, L3, L4. These three vertebrae make up the middle of the lumbar spine.
- L5. This is the last vertebra of the lumbar spine and the one that connects the spine to the sacrum (a wedge-shaped bone connected to the pelvis and responsible for supporting the weight of the spine).
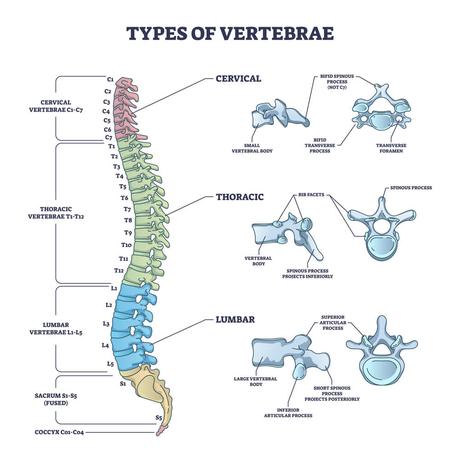
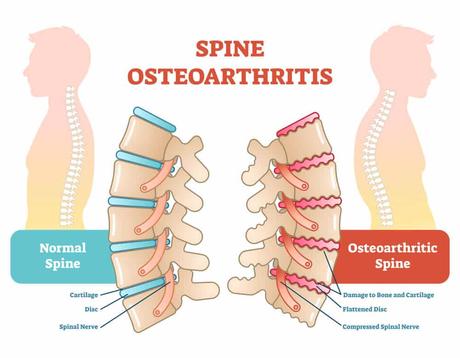
The vertebrae in the lumbar spine are the largest ones in the spinal column because they bear most of the weight of the body and external loads. Between each pair of vertebrae is a rubbery pad made of cartilage – known as intervertebral disc – which enables movement flexibility and protects the bones from shock and friction damage.
As we’ll see below, most people’s intervertebral discs degenerate over time, with 90% of people aged 60 and over showing some degree of disc degeneration. Today, lumbar disc degenerative disease is believed to be the leading cause of low back pain worldwide.

Another unique aspect that characterizes the vertebrae of the lumbar spine is that, unlike the vertebrae of the cervical and thoracic spine, the spinal cord does not run through most of them. The spinal cord acts as a “highway” for nerve signals: it coordinates reflexes, transfers motor commands from the brain to the body, and sends information regarding sensations from the body to the brain.
The spinal cord stems from the brain and, as it travels through the spine, branches spread out to all regions of the body. At the lower end of the spinal cord is the cauda equina, a group of nerves and nerve roots spread through the lower body. These nerves are responsible for providing motor and sensory innervation to the bladder, anus, perineum, and legs.
At the vertebra L1 or L2, the true spinal cord ends. In the subsequent sections, axons of nerves begin to exit the cauda equina to the left and right sides of the body. In particular, the L3 spinal nerve roots exit the spine through small bony openings (known as intervertebral foramina). This nerve is responsible for transferring motor and sensory signals to specific areas of the lower body:
- Areas of the skin at the front of the thigh and inner leg. The L3 dermatome refers to the area of the skin that is innervated by the L3 spinal nerve. This area extends to the lower back, inner thighs, and inner legs (below the knees).
- Muscles in the hip, thigh, and leg. The L3 myotome is the group of muscles controlled by the L3 nerve. These are located in the hip, thigh, and leg.
The L3-L4 motion section (which is a section composed of two vertebrae and their intervertebral disc) is also responsible for protecting delicate structures of the lower spine, including the cauda equina.
Potential Problems and Injuries Involving the L3
The lumbar spine is the most commonly injured section of the spine. – The L3 is susceptible to injuries and wear and tear. The reason for this lies in the fact that this vertebra is regularly called to withstand exceptional loads and rotatory strain.
Not only is the L3-L4 section of the spine one of the most common sites of chronic back pain, and injuries here can compromise spinal health.
Some of the most common conditions affecting the L3 and the lower spine as a whole include:
Osteoarthritis
Osteoarthritis (OA) is a degenerative joint disease characterized by the gradual breakdown and eventual loss of the joint cartilage, which is a cushion-like layer responsible for helping the vertebrae move with as little friction as possible.
When this occurs in the spinal region it is identified as spinal osteoarthritis. This condition affects the cartilage that lines the facet joints, which are the places where your vertebrae meet to create a motion segment.
Spinal OA can affect any facet joint in the spine, but it’s more common in the cervical and lumbar spine, where vertebrae are subject to ongoing rotational strain and overload.
Although anyone can suffer from osteoarthritis during their lifetime, it is important to note that certain risk factors will significantly increase the risk of suffering from degenerative conditions.
These include repetitive stress on the spine, age, sex, tobacco use, old and new injuries, and suffering from obesity (due to the excessive strain placed on the spine). We’ll talk more about the causes of L3 injuries below.
Degenerative Spondylolisthesis
Degenerative spondylolisthesis is a condition that develops due to the natural, age-related wear and tear on your spine’s joints and ligaments. This wear and tear weakens the structures in and around the vertebrae, allowing one vertebra to slide forward over the one below.
The lower back – and, in particular, the L3-L4 motion section – is the spinal segment most commonly affected by this condition. This is because your low back is constantly under significant loads and strains, due to its pivotal role in supporting your upper body, bending, and rotating.
When degenerative spondylolisthesis occurs at this L3 level, it causes the L3 vertebra to slip forward and over the L4 vertebrae, leading to complications such as:
- Compressed spinal nerves
- Limited mobility in the lower body
- Disruption of bowel or bladder function due to irritated nerves
- Nerve root irritation leading to weakness in lower limbs
- Progressive misalignment of the vertebrae involved
- Increased risk of injuries and spinal fractures
- Increased risk of spinal stenosis (the narrowing of the spinal canal, which causes consequent damage to the spinal nerves).
- Heightened risk of osteoarthritis, due to the fact that areas of the vertebrae will place excessive loads on the facet joints
- Increased risks of intervertebral disk injuries
Degenerative spondylolisthesis has been seen to be present in nearly 14% of people with chronic lower back pain in a study conducted in 2013.
Sacralization
Sacralization is a congenital condition where the L5 vertebra, the lowest lumbar vertebra, fuses with the sacrum, the base of the spine. When this happens, it affects the usual structure of the lower back, often leading to a redistribution of stress and loads across other lumbar vertebrae, including the L3 vertebra.
The excessive, undue load on this and other vertebrae of the lower spine can intensify wear-and-tear damage and increase the risk of injuries on the “non-fused” components of the lower back.
Cysts
Cysts are noncancerous, closed pockets of tissue that can be filled with fluid, pus, or other material. Their cause is unknown, but they may develop as a consequence of degenerative changes or repetitive motions of the joints.
Besides leading to pain and discomfort, cysts can also cause nerve compression by narrowing the spinal canal (which houses the spinal cord) and the intervertebral foramina (the openings through which nerve axons exit the spinal cord and cauda equina).
Patients with spinal cysts often also have other conditions of the spine, like arthritis or disc disease. Although they are most commonly found at the L4-5 level, which is the site of maximum mobility of the spine, they can occur anywhere in the spine and lower back.
Despite their benign nature, these cysts can significantly impact your spinal function and quality of life. Additionally, since some cancers can cause cysts, they should be immediately examined by a specialist.
Fractures
Fractures in the lumbar spine can have catastrophic consequences on your spinal health and mobility. They can range from minor cracks to complex fragmentary breaks (which occur when fragments of the bone become entirely detached) and cause damage to surrounding spinal structures, including nerves and ligaments. Besides pain and discomfort, spinal structures can lead to long-term spine instability and reduced range of motion.
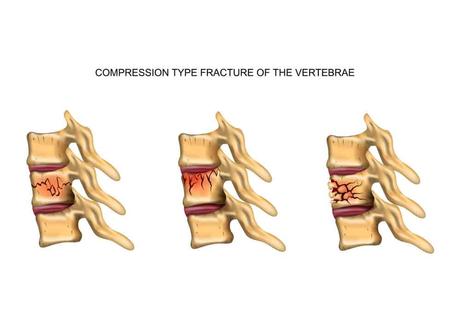
Typically, this injury is caused by sudden, forceful movements or due to excessive loads. Although car accidents often cause spinal injuries, it is important to note that a leading cause of vertebral fractures is undiagnosed osteoporosis.
Many patients don’t realize they have osteoporosis until a fracture occurs – and some estimates show that the prevalence of osteoporotic vertebral fractures in aging women with acute lower back pain is as high as 76.5%!
Be sure to undergo the necessary screenings to evaluate your bone mineral density and take steps to prevent osteoporotic vertebral fractures.
Causes of L3 Injuries
L3 injuries can stem from multiple causes – as well as from a combination of risk factors, such as lifestyle choices, genetics, and even how physically demanding your job is.
- Traumatic injury. Experiencing a sudden, unexpected load or force can cause fractures or strains in the L3 area of the spine. These occur if, for example, you are involved in a car accident – but can also happen due to non-contact trauma, such as lifting a heavy object or performing a forceful movement while playing sports.
Estimations show that nearly 80% of soccer players, 30% of American football players, 95% of hockey players, and almost 90% of baseball players experience low back pain due to lumbar spine injuries throughout their careers. - Repeated stress on the spine. If your job or sport involves regular, forceful movements that place excessive strain on the spine, you are more likely to experience spinal injuries and degenerative conditions. This is because repeated stress can speed up the wear and tear of essential spinal components, such as the L3-L4 intervertebral disc.
Ongoing stress on the spine can also increase the risks of cysts and inflammation, which narrow the space in and around the spinal canal and intervertebral foramina, leading to nerve irritation and damage. - Lifestyle factors. Your habits and lifestyle can weigh in on your risk of developing spinal injuries and degenerative diseases. For example, poor posture, frequent bending and lifting, using tobacco products, and insufficient physical activity can speed up the rate of degeneration and weaken your spine, thus increasing the risk of injuries.
- Obesity. Obesity and being overweight have long been associated with a heightened risk of low back pain and lumbar spine injuries. As we’ve seen above, the lower back – including the L3 vertebra – is the segment of the spine called to withstand the highest loads and support the weight of the rest of the spine.
The additional strain placed on the lower back by excess weight can speed up the rate of disc degeneration and make injuries more likely. Plus, obesity is a risk factor for metabolic disorders, inactivity, and mental health disorders, all of which can contribute to heightened chronic pain. - Age. Although anyone can suffer from back pain at any time during their lifetime, age-related deterioration of intervertebral discs and other spinal components can make injuries more likely. It is estimated that up to 70% of older adults suffer from back pain to some extent. It is also worth noting that other conditions associated with aging – like low bone mass density and osteoporosis – can increase the risk of injuries like fractures.
Your spine health can also be compromised by benign or malignant growths of tissue (e.g.: tumors) pressing on the L3, as well as years of poor posture and lifestyle choices.
Symptoms of L3 Injuries
The lumbar spine and the nerves that stem from the cauda equina play a vital role in controlling communication between the lower part of the body and the brain. Injury or degeneration that affects the L3 and adjacent vertebrae may compress, irritate, or damage the L3 spinal nerve.
Subsequently, this impacts all areas connected by the L3 spinal nerve: the hips, groin, thigh, and abdominal muscles.
Depending on the extent of the damage, nearby nerves, such as the sciatic nerve, can also be affected, thus impacting a whole host of body functions, including lower limb mobility and bladder and bowel control.
Some of the symptoms indicating that your lower back pain may be related specifically to the third lumbar vertebra include:
- Sharp pain or numbness in the thigh and/or inner part of the leg. The L3 dermatome (the area of the skin innervated by the L3 spinal nerve) extends to the thigh and inner part of the leg. When the communication between these areas and the brain is cut off, nerve signals relating to pain, touch, vibration, and temperature are disrupted.
This can cause you to experience numbness or, alternatively, sharp pain in response to stimuli that should normally be painless or cause only mild discomfort. These conditions are known as allodynia and hyperalgesia, respectively. - Thigh and/or knee weakness. The L3 spinal nerve also controls the movement of groups of muscles around the thigh and knee (L3 myotome). When the nerve connection is impacted, you may experience instability, weakness, and involuntary movements, such as cramps and spasms.
- Abnormal sensations, such as a feeling of pins and needles and/or tingling. Nerve damage or irritation is often associated with abnormal sensations, such as tingling or pins and needles, a condition known as paresthesia.
- Loss of bowel or bladder control. If the nerves of the cauda equina are affected this can cause numbness or pain in the genital or rectal areas, inability to urinate or defecate or urinary or bowel accidents. If these symptoms occurs, you need to seek medical attention right away as this indicates severe nerve injury and likely requires urgent surgery.
Injury to the third lumbar vertebra may also cause pain, discomfort, reduced range of motion, and instability in the lower spine. While the location of the pain can tell you more about what section of the spine is affected, it is important to seek an accurate diagnosis. Without prompt intervention, L3 injuries can lead to complications such as mobility issues, chronic pain, and disability.
Treatments for L3 Injuries
Despite how common low back pain is, most people struggle to find an accurate diagnosis of their condition – and, even more worryingly, are unable to access treatment plans that are both effective and sustainable in time. A 2019 study even reports that low back pain accounts for the highest global burden of disease related to years lived with disability worldwide.
Navigating the different treatment options isn’t easy – but estimations show that 76-90% of patients with acute or persistent low back pain fully recover. Below, we’ll look at the different treatment options available today.
Surgical Treatments
Given the risks, side effects, and lengthy recovery periods associated with back surgery, this is often regarded as the last option, usually after more conservative therapies have failed or in the case of advanced L3 or cauda equina nerve damage.
- Microdiscectomy. This surgical procedure involves performing a small incision to remove problematic disc material, such as in the case of a herniated or bulging disc that is compressing nerves around the L3 vertebra. Although it’s minimally invasive, it can lead to complications like infection, nerve damage, or recurrence of disc herniation.
- Laminectomy. This is a type of spinal surgery aimed at expanding the spinal canal by removing or trimming the lamina (the roof of the spinal canal). It can offer pain relief if the spinal canal has narrowed or is disrupted and is impacting the spinal nerves. Potential risks include infection, bleeding, and nerve injury.
- Foraminotomy. This surgical procedure enlarges the opening where nerve roots leave your spinal canal (the intervertebral foramina), easing neural pressure and preventing permanent damage. Complications include nerve injury, infection, and the possibility of the foramen narrowing again.
- Facetectomy. In this surgery, parts or all of a facet joint are removed to decrease pressure on the spinal nerves. This surgical procedure, while generally successful, could lead to complications including nerve damage, infection, and spinal instability.
- Fusion of L3-L4. This procedure aims to reduce pain, inflammation, and spinal instability by fusing together two vertebrae. In practice, it involves removing both the intervertebral disc and the damaged joint components. Spinal fusion can limit your range of motion and it doesn’t always fully ease the pain.
- Lumbar artificial disc replacement. This surgery involves the removal of a damaged disc, which is then substituted with an artificial one. Although this procedure allows the patient to retain some degree of mobility while reducing pain and inflammation, it can lead to risks like prosthetic breakdown, infection, and recurring symptoms.
More and more people are opting for surgery to resolve their back pain. However, it’s important to keep in mind that while surgery may help with back pain caused by neural damage, infection, or cancer, there’s no evidence that it can help with non-specific low back pain. In other words, undergoing surgery to ease your L3 vertebra pain may not just be incredibly risky – but also ineffective.
Non-Surgical Treatment Options
Non-surgical treatment options are often the go-to approach for people experiencing L3 and lumbar back pain in general. However, some of these treatments may be ineffective at best and damaging to your health at worst.
Because of this, it’s paramount to find an option that is as efficient in relieving pain as it is safe and conducive to overall, long-term musculoskeletal health. Let’s look at the options you have below.
- Medication/drugs. Drugs like anti-inflammatories, NSAIDs, muscle relaxants, nerve pain medications, or opioids are commonly employed to relieve L3 spinal pain.
However, if you are struggling with chronic back pain, taking these medications daily can expose you to a multitude of side effects, including a heightened risk of heart attack and stroke, stomach ulcers, kidney disease, lethargy, addiction, and overdose. Nearly 20% of people with back pain are prescribed opioids as standard today. - Immobilization. This strategy usually involves the use of a back brace or cast to align the spine and aid healing. Although this can help relieve pain at first and prevent further injuries, long-term use could lead to muscle weakness, potentially complicating the healing trajectory.
- Physical therapy. Physical therapy can help you strengthen the muscles of your back, restore mobility, and improve your posture through techniques like thermal therapy, stretching, and strength training. Physical therapy is usually part of a multi-disciplinary approach to improve spinal health.
- Chiropractic. This approach focuses on realigning your spine through manipulation to restore function. It isn’t equally efficient for all patients and could be unsuitable for those with conditions such as osteoporosis or spinal instability.
- Injection. Nerve blocks, epidurals, and corticosteroid injections introduce pain-relief drugs directly to the affected area to curb severe pain. They work by reducing inflammation or blocking the actions of nerves responsible for carrying pain signals.
Although they have a longer-lasting effect (2-3 months) compared to normal pain-relieving drugs, these therapies carry risks such as infection, bleeding, and accidental delivery of the drug into the bloodstream. - Regenexx. Regenexx® uses research-based orthobiologic procedures and patient protocols that provide a non-surgical, non-pharmaceutical alternative for patients with a range of orthopedic disorders, including back pain, joint injuries, and osteoarthritis.
It works by concentrating the patient’s own cells and healing platelet growth factors to apply them precisely to the injured area, thus kickstarting the body’s ability to heal naturally and regenerate damaged tissues.
Regenexx doctors take a thorough history, perform a complete physical examination, and directly review patient imaging to obtain an accurate diagnosis. .They also use a comprehensive treatment approach called the functional spinal unit (FSU) treating functional spinal unit (regenexx.com) which address all of the damaged tissues that lead to pain and dysfunction.
This approach provides better and longer results compared to simple injection to 1 area and our outcomes are tracked here Regenexx Patient Outcome Data | Centeno-Schultz Clinic (centenoschultz.com)
Learn the Anatomy of the Spine to Avoid Injuries
The spine is a highly complex and interconnected system: your thoracic spine protects your lungs and heart, and provides attachment points for multiple essential muscles; the cervical vertebrae support your head and keep the neck flexible; lastly, your low back ensures support, stability, and unrestricted range of movement.
Given how interrelated this system is, when looking to address a problem with your L3 or avoid injuries, you’ll need to have a better understanding of how your spine works and opt for a whole-person approach that is truly conducive to long-term spinal health.
Learn more about Regenexx.
Click Here
