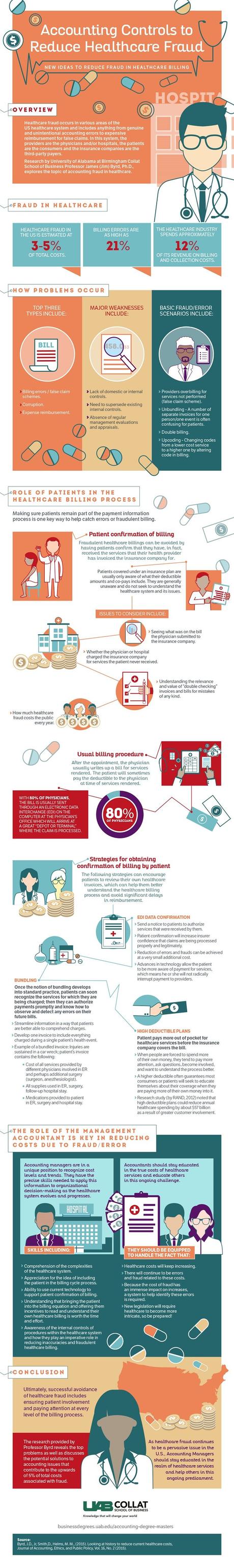
There are a lot of costs involved in healthcare these days, as we all know, but not all of these costs are justified. Because of the insurance system and the lack of involvement with the patients when it comes to insurance payments, many healthcare providers end up getting paid more than they are actually owed. This can happen both by accident or on purpose, but the result is the same: it has a negative impact on the cost of healthcare and patient trust in healthcare organizations.
There are times when the complicated healthcare system results in unintentional billing errors, which results in the insurers paying more. Sometimes, it’s more malicious. The hospital can end up billing for services that the patient didn’t receive. This is often easy to do because the bill gets sent directly to the insurer, without the patient confirming that everything in the bill is correct. The best way to confront the widespread fraud issue is to have the patient involved in the process; they are the first line of defense when it comes to identifying billing errors.
In a professional capacity, it’ll be accounting managers who are in the best position to help combat these problems. They can help improve internal procedures, encourage patients to engage with the billing side of healthcare, and can spearhead the use of technology to make the billing process more straightforward and transparent.
To learn more about this, take a look at the infographic from the University of Alabama Birmingham outlined below.
Infographic design by University of Alabama Birmingham University of Alabama Birmingham
This post was a collaboration.

