You’ve all heard of “superbugs,” bacteria that are resistant to most, if not all, of medical science’s antibiotics. See, for example:
- Alarming: Outbreak of antibiotics-resistant “nightmare bacteria” in Chicago
- Antibiotics-resistant superbug kills 2, infects 180 in Los Angeles
Bacteria are evolving beyond our antibiotics because of our profligate, over-prescription, and indiscriminate use of antibiotics, especially by the corporate meat industry’s dumping of antibiotics (and hormones too) into the feed of factory farm animals.
Here’s another sign that our antibiotics are losing their ability to combat infections.
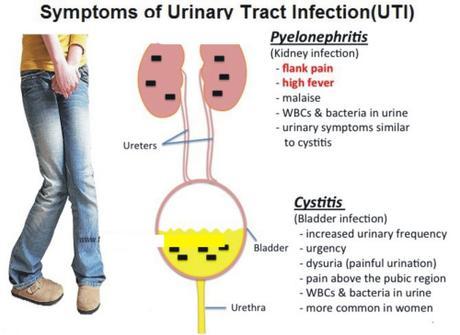
Urinary tract infections, the most common bacterial infections in the United States, increasingly are resistant to oral antibiotics.
Rita Rubin writes for WebMD Health News, April 29, 2015, that doctors are running out of oral antibiotics to treat such urinary tract infections (UTI), which account for nearly 10 million annual visits to doctors’ offices or hospital emergency departments.
That’s happening as the bacteria causing them become more resistant to the medicines used to treat them. Antibiotic resistance in general is on the rise worldwide, but one especially troubling example is the rise in resistant strains of E coli, the bacteria that cause more than 80% of UTIs.
In some cases, doctors have had to resort to older, less-effective antibiotics. In other cases, they’ve had to put a catheter into patients’ arms to give antibiotics through a vein, because no medications taken by mouth worked. Sometimes doctors have had to ask the FDA for permission to use a medicine that the agency has not yet approved.
“Bacteria are smarter than humans,” says Lilian Abbo, MD, an infectious disease specialist at the University of Miami. “When you challenge bacteria with an antibiotic, maybe the first time the bacteria will say, ‘Oops, we’ve never seen this,’ and the antibiotic will kill them.”
But familiarity with antibiotics breeds contempt in bacteria, which can develop ways to make them ineffective. Resistance can even spread among bacteria, enabling them to fend off antibiotics they’d never previously been exposed to.
Sometimes, doctors must try two, three, or even four antibiotics to vanquish stubborn UTIs, Abbo says. As an infectious disease specialist, she sees patients who keep getting UTIs. Those fourth-line medications are often “broad-spectrum” antibiotics, meaning they also wipe out the good bacteria in the gut that help with digestion and your immune system.
“We’re basically using a grenade to kill a mosquito,” Abbo says. “The mosquito became resistant to all the repellents and keeps biting you.”
One study of E. coli taken from urine samples of U.S. patients found that the greatest increases in resistance between 2000 and 2010 were for the antibiotics Cipro (3% to 17%) and Bactrim (18% to 24%). (Bactrim is also called Sulfatrim and Septra).
A third of women will get a UTI that needs to be treated with an antibiotic by age 24. Half of all women get at least one UTI in their lifetime. If you’re one of them, you’re familiar with the symptoms — the painful peeing and the frequent, urgent feeling that you have to go to the bathroom. Untreated, UTIs can lead to a kidney infection that could cause serious or permanent damage.
Because of safety concerns, pregnant women have even more limited choices when it comes to treating UTIs, which are common during pregnancy. Along with kidney infections, UTIs can also cause preterm labor. At the same time, some antibiotics prescribed for the infections could hurt the unborn baby, says Catherine Eppes, MD, MPH, an obstetrician-gynecologist at the Baylor College of Medicine in Houston.
In a paper published in March in the American Journal of Obstetrics & Gynecology, Eppes and colleague Steven Clark, MD, described a 31-year-old patient who was 12 weeks pregnant and having fever, nausea, and pain due to a UTI.
She’d been treated 2 weeks earlier for another UTI with Macrobid, a commonly prescribed older antibiotic. This time, she was hospitalized and prescribed Rocephin. On the third day, tests showed that her infection was resistant to that antibiotic. She was switched to one given through a vein. After 2 days in the hospital, she was discharged but had to keep getting the antibiotic by IV for 12 more days at home.
“We seem to be getting more and more women admitted to our hospital service with these infections,” Eppes says. “Antibiotic resistance, especially in UTIs, is definitely an emerging and important issue.”
In some cases, no antibiotic is effective against postmenopausal women’s symptoms, because they don’t actually have a UTI. “Such women come back in time and time again with those symptoms,” suggesting that their symptoms are due to age-related hormonal changes, not an infection, says Thomas Hooton, MD, He’s a University of Miami infectious disease doctor who specializes in treating people who keep getting UTIs.
One thing contributing to antibiotic resistance in the treatment of UTIs is that some people with no symptoms are getting prescriptions, Hooton says.
For example, healthy women typically provide urine samples at checkups so the doctor can look to see whether the samples have protein or sugar, either of which could be signs of underlying problems. Sometimes, though, white cells, a sign of inflammation, turn up in the test results, and doctors go ahead and prescribe an antibiotic, Hooton says, even though having bacteria in the urine without any symptoms isn’t a disease, but the doctors mistakenly think that symptoms will arise if the apparent infection isn’t quashed. In people without symptoms, antibiotics are appropriate only for pregnant women whose urine suggests they might have a UTI, Hooton says.
~Éowyn

